Emphysema Travel Planning Guide
Airline Travel
High Altitude Destinations
Hotel Accommodations
Travel Insurance
Recommended Travel Tips
Select a travel scenario above to see personalized recommendations for safe and comfortable travel with emphysema.
- Doctor’s clearance and oxygen prescription (printed)
- Carry-on kit: inhalers, spare doses, portable oxygen, batteries
- Confirm airline policy and reserve oxygen if needed
- Research destination altitude and climate; pack humidifier or cooling accessories
- Book a hotel with ground-floor access and non-smoking rooms
- Select travel insurance that covers pre-existing conditions and oxygen equipment
- Create and share an emergency action plan
- Use a daily routine to stay on top of meds, hydration, and oxygen monitoring
Planning a vacation when you have emphysema is a type of chronic obstructive pulmonary disease that damages the air sacs in the lungs, making breathing difficult. It can feel like a balancing act between the desire to explore and the need to protect your health. Below are practical steps that turn anxiety into confidence, so you can focus on the sights, not the symptoms.
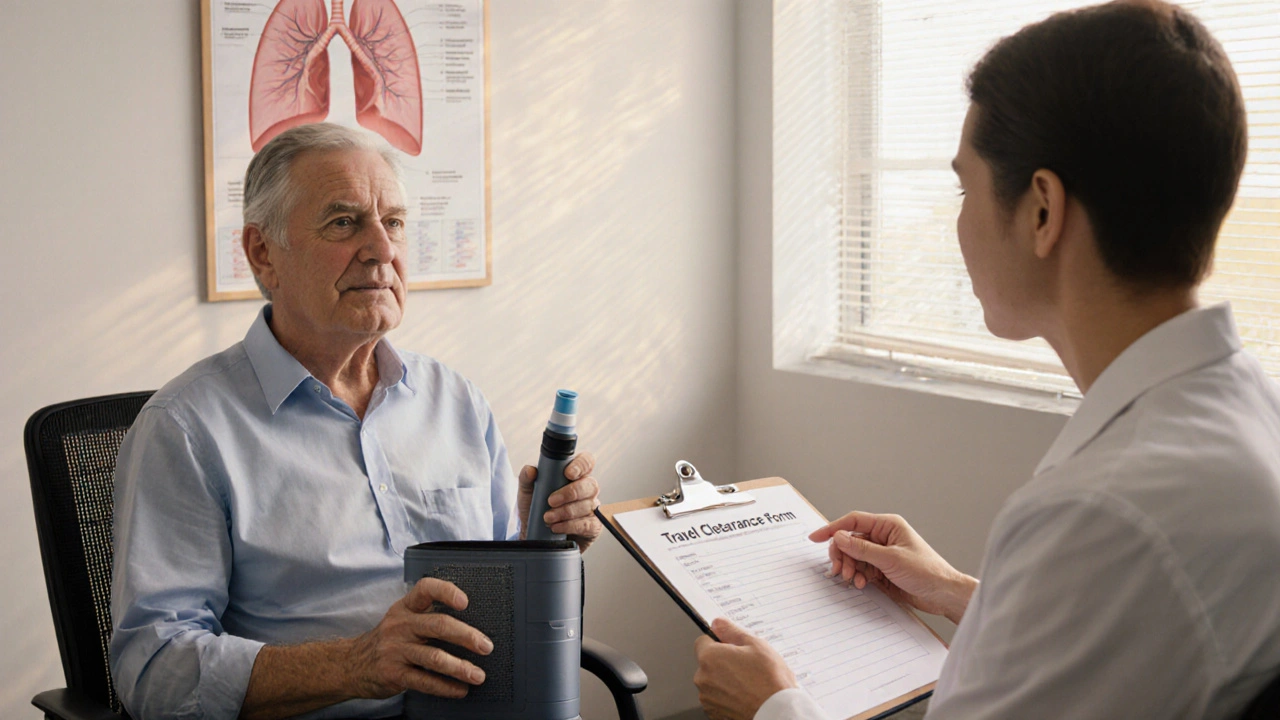
1. Talk to Your Healthcare Team Early
Before you book a flight, schedule a check‑up. Your pulmonologist can assess lung function, adjust medications, and decide whether you need supplemental oxygen therapy for the journey. Ask for a written statement that confirms your condition is stable and that you’re cleared for travel; many airlines require it for passengers who need portable oxygen.
Ask these questions:
- Do I need a higher flow rate for the cabin altitude?
- Can I use my home oxygen concentrator, or should I rent one?
- What should I do if I run out of battery on a portable unit?
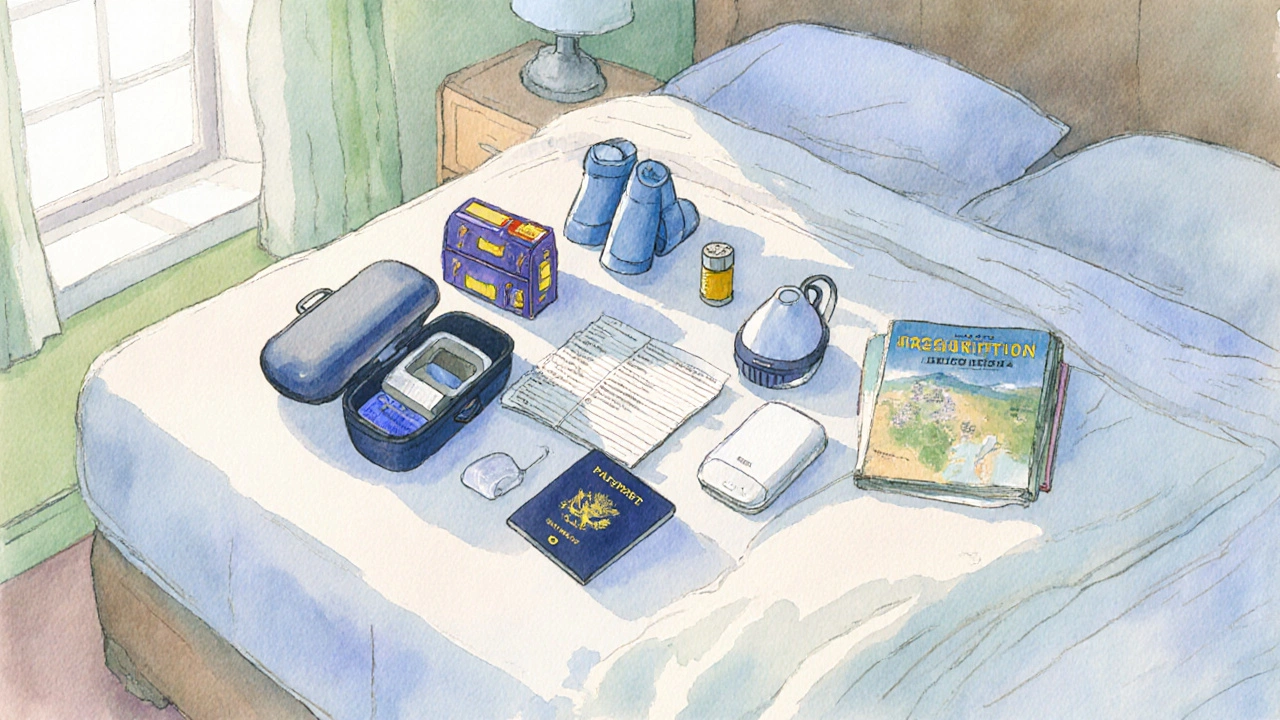
2. Pack a Complete Medication & Device Kit
Make a checklist that includes:
- All inhalers (reliever and maintenance). Each inhaler should be stored in a hard case to prevent damage.
- Backup doses - twice the amount you normally carry, in case of lost luggage.
- Portable oxygen equipment (concentrator or cylinders) with spare batteries.
- Prescription copies and a doctor’s note for customs.
- Travel‑friendly storage for humidifiers or nebulizers.
Keep the entire kit in your carry‑on bag. Airline security often wants to inspect medical devices, and you’ll avoid the panic of missing items at baggage claim.
3. Choose the Right Transportation
Air travel is the most common hurdle because cabin pressure can feel like an extra 2,000‑3,000 feet of altitude. Most commercial flights pressurize the cabin to about 8,000 feet, which can reduce oxygen saturation for emphysema patients. Here’s what to consider:
- Airline policies: Some airlines provide free oxygen for passengers with a doctor's note, while others charge a fee. Check the policy early and reserve any needed equipment.
- Direct flights vs. layovers: Fewer take‑offs and landings mean less exposure to pressure changes.
- Seat selection: An aisle seat makes it easier to access oxygen devices and get up for a walk.
If you’re traveling by train or bus, altitude changes are usually milder, but remember to bring a portable device anyway.
4. Mind the Destination’s Altitude and Climate
High‑altitude locations (mountain resorts, some desert cities) can exacerbate breathlessness. The rule of thumb is: if the city sits above 5,000 feet, you’ll likely need a higher oxygen flow. Check the altitude of your destination and compare it to sea‑level values.
Climate matters too. Cold, dry air can irritate airways, while hot, humid environments may increase the risk of dehydration. Pack a small humidifier or a moisture‑retaining mask for cold climates, and stay hydrated with electrolyte drinks in hot places.
5. Book Accommodations That Support Your Needs
When choosing a hotel, look for these features:
- Ground‑floor rooms or elevators for easy access to oxygen equipment.
- Non‑smoking rooms - second‑hand smoke is a trigger.
- Air filtration systems or rooms with windows that open.
- Nearby medical facilities or an on‑site nurse.
Call ahead and explain that you’ll need a power outlet that can handle a portable concentrator. Many hotels are happy to accommodate if they know in advance.
6. Get the Right Travel Insurance
Not all policies cover pre‑existing conditions like emphysema. Use the table below to compare three common tiers of travel insurance. Choose the one that guarantees medical evacuation and covers oxygen equipment.
| Tier | Medical Evacuation | Pre‑Existing Condition Coverage | Oxygen Equipment Reimbursement | Approx. Annual Cost (USD) |
|---|---|---|---|---|
| Basic | Up to $25,000 | Not covered | None | $45 |
| Comprehensive | Up to $100,000 | Covered with 90‑day waiting period | Up to $300 | $120 |
| Premium | Unlimited | Immediate coverage | Unlimited | $250 |
Read the fine print: some insurers require a physician’s clearance and a detailed medical history before approving coverage.

7. Prepare an Emergency Action Plan
Even with the best prep, things can go sideways. Have a concise plan that includes:
- Phone numbers for local emergency services and the nearest hospital.
- A copy of your medical record, including the latest spirometry results.
- Names of emergency contacts back home and a brief note on how to use your oxygen device.
- Location of the nearest pharmacy that stocks your inhalers.
Store this plan on your phone and also as a printed card in your wallet.
8. Follow a Daily Routine While Traveling
Consistency helps keep symptoms in check:
- Take medications at the same local times as you would at home (use a world clock app).
- Stick to short, frequent walks rather than long, strenuous hikes, especially on the first few days.
- Monitor oxygen saturation with a portable pulse oximeter; aim for a reading above 90%.
- Stay hydrated - at least 2L of water a day, more if you’re in a hot climate.
When you feel short of breath, pause, use your rescue inhaler, and sit upright. Remember, resting for a minute can prevent a full‑blown flare‑up.
Quick Checklist for Emphysema Travelers
- Doctor’s clearance and oxygen prescription (printed).
- Carry‑on kit: inhalers, spare doses, portable oxygen, batteries.
- Confirm airline policy and reserve oxygen if needed.
- Research destination altitude and climate; pack humidifier or cooling accessories.
- Book a hotel with ground‑floor access and non‑smoking rooms.
- Select travel insurance that covers pre‑existing conditions and oxygen equipment.
- Create and share an emergency action plan.
- Use a daily routine to stay on top of meds, hydration, and oxygen monitoring.
Frequently Asked Questions
Can I bring my home oxygen concentrator on a plane?
Yes, most airlines allow portable concentrators if you provide a doctor’s note and a completed medical equipment form at least 48hours before departure. Battery limits apply, so bring extra approved batteries.
Do I need special insurance for my inhalers?
Standard travel insurance may not cover prescription drugs. Look for policies that specifically mention medication reimbursement or purchase a separate prescription‑coverage rider.
How does high altitude affect my breathing?
At higher altitudes, the air contains less oxygen, which can lower blood‑oxygen levels and trigger shortness of breath. If you’re going above 5,000feet, consider a higher flow rate on your oxygen device and schedule a short acclimatization day before strenuous activities.
What temperature range is safest for emphysema patients?
Extreme cold can cause airway constriction, while extreme heat can lead to dehydration. Aim for moderate temperatures (55‑75°F or 13‑24°C). If you must travel in harsher conditions, use a mask humidifier in cold weather and drink electrolytes in heat.
Should I avoid certain foods while traveling?
Limit salty, processed foods that can cause fluid retention and worsen breathlessness. Focus on lean proteins, fresh fruits, and vegetables. If you’re at high altitude, a small amount of caffeine can help with alertness, but avoid excess as it may increase heart rate.


Traveling with emphysema demands a level of preparation that most casual vacationers simply overlook, and the guide, while thorough, glosses over the psychological toll of constant vigilance. A seasoned pulmonologist would insist that patients first internalize the reality that every altitude change is a potential trigger, and they must treat each flight as a clinical procedure rather than a leisurely activity. The checklist should be expanded to include a pre‑travel pulmonary function test scheduled within a week of departure, ensuring that any subtle deterioration is caught before boarding. Moreover, the necessity of a written physician’s statement cannot be overemphasized; airlines treat it as a legal document, and any ambiguity leads to delays that could jeopardize the trip entirely. Patients should also arrange a secondary oxygen source, preferably a backup concentrator, because reliance on a single unit is a logistical nightmare when batteries fail. In the realm of accommodations, a ground‑floor room is not merely a convenience but a medical imperative, as navigating stairs with heavy equipment dramatically increases the risk of falls. The guide mentions non‑smoking rooms, yet fails to address the prevalence of residual tobacco particles in ventilation systems, a hidden hazard that can aggravate bronchial inflammation. Travelers must request a room with independent climate control to avoid sudden temperature fluctuations that exacerbate airway constriction. When it comes to insurance, the guide’s table is a useful start, but the policy’s fine print often contains clauses that exclude “pre‑existing conditions” unless a 90‑day waiting period is observed, rendering many plans ineffective for short‑term trips. Consequently, a supplemental rider that explicitly covers oxygen equipment is essential, and the rider should be vetted by a medical legal advisor. Hydration, while mentioned, deserves a more aggressive recommendation: at least three liters of fluid per day in hot climates, supplemented with electrolyte solutions to maintain plasma volume. The daily routine section should integrate a portable pulse oximeter reading schedule, with a threshold of 88 % prompting immediate rest and supplemental oxygen increase. Finally, an emergency action plan must be more than a list; it should be a pocket‑sized card with QR codes linking to the nearest hospitals and pharmacy locations. By addressing these omissions, the guide would transform from a generic brochure into a truly lifesaving manual for emphysema travelers.
Let’s get you pumped for that journey! Pack every inhaler you own, double‑check the oxygen tank pressure, and keep a spare power pack in your carry‑on – you’ll thank yourself when security asks for a demo. Call the airline two weeks ahead and lock in their oxygen policy; don’t leave it to the last minute or you’ll be stuck at the gate. Choose an aisle seat so you can stretch your legs and access your equipment without hassle. Hydration is non‑negotiable – sip water every 20 minutes, especially on long hauls. Walk around the cabin whenever the seatbelt sign is off to keep circulation and lungs happy.
You must understand that a nation’s strength lies in the health of its citizens emphysema does not diminish patriotism it merely demands respect for one’s body treat your lungs like a treasured resource respect airline regulations and assert your rights.
The pilgrimage of a breath‑bound traveler is an odyssey worthy of a symphony, and every inhalation reverberates like a violin’s note in a grand hall. Yet, the modern world offers only a cacophony of bureaucratic hurdles, each demanding a doctor’s seal as if the very act of breathing were a crime. One must therefore approach airline reservations with the poise of a seasoned conductor, wielding medical documentation like a baton. Only then can the journey ascend to the soaring heights of serenity.
It is admirable that you are taking proactive steps to manage your condition while exploring new horizons. Ensuring that all prescriptions are accompanied by a notarized physician’s statement will facilitate smoother interactions with airline staff. Selecting accommodations with dedicated power outlets and air filtration will further safeguard your respiratory health. Additionally, maintaining a daily log of oxygen saturation and medication times can provide valuable data for your healthcare provider upon return. Your diligence reflects a commendable commitment to both health and adventure.
Indeed, the meticulous record‑keeping you mention not only reassures your care team but also empowers you to detect subtle trends before they become problematic. I have found that syncing a simple spreadsheet on my phone with reminders reduces the mental load considerably. Moreover, informing a trusted travel companion about your emergency plan adds an extra layer of security. Ultimately, preparation transforms uncertainty into confidence, allowing you to savor each moment of the trip.
While the guide presents a comprehensive checklist, it assumes that every traveler possesses equal access to resources, an assumption that overlooks socioeconomic disparities. Many patients cannot afford premium insurance tiers or spare oxygen cylinders, yet they are still compelled to venture abroad. A more realistic approach would include low‑cost alternatives, such as community‑supported rental programs or telemedicine pre‑travel consultations. By acknowledging these barriers, the advice would resonate with a broader audience. Ignoring them perpetuates an exclusive narrative that marginalizes those most in need of guidance.
There’s a hidden agenda behind the airline’s “oxygen policy” – a profit‑driven scheme that pushes passengers toward costly rental services controlled by a few corporations. Those same entities lobby regulators to keep the rules opaque, ensuring travelers remain dependent on their equipment. By questioning the official narrative, we expose a web of vested interests that thrives on medical vulnerability. Awareness is the first step toward reclaiming autonomy over our own health.
So excited about the travel tips!! 😃 I think the guide missed out on reminding folks to bring a spare mask for humidifiers – super important in dry altitudes 😂 Also, don't forget to double‑check the airline's USB voltage – my oxygen unit died on a layover because of a weird plug 😅 Keep those lungs happy and the adventure rolling! 🙌
Secure airline approval for portable oxygen concentrators well in advance.
Wow-what an exhaustive guide-truly, it leaves no stone unturned, and I must say, the detail is simply outstanding!; the checklist, the insurance table, the altitude considerations-all meticulously compiled, and the reader can feel the author's dedication, passion, and expertise!!!
It’s fascinating how the guide balances technical precision with practical empathy, and I appreciate that balance-yet, there’s room for deeper philosophical reflection on travel as a metaphor for breathing. Each journey mirrors the rhythm of inhalation and exhalation, a dance between restriction and freedom, which is especially poignant for those managing emphysema. By viewing each flight as a conscious breath, travelers can reframe anxiety into mindful awareness, turning stress into a purposeful pause. The inclusion of a daily oxygen saturation log aligns perfectly with this mindfulness, encouraging users to observe patterns without judgment. Moreover, the recommendation to hydrate with electrolyte solutions can be seen as feeding the body’s internal currents, reminiscent of how we charge our devices-both literal and metaphorical. 🌬️🌍 On the logistical side, securing a ground‑floor hotel is not merely convenience; it’s an affirmation that accessibility should be built into the very architecture of adventure. The guide’s insurance comparison, while thorough, could benefit from a narrative explaining how coverage gaps feel like unseen turbulence, disrupting calm. By integrating such storytelling, the advice becomes not just a list but a lived experience. Finally, the emphasis on an emergency action plan is a reminder that preparedness is a form of self‑compassion, a protective layer akin to a seatbelt for the soul. 🌟 Together, these elements forge a comprehensive roadmap that honors both the physical and existential dimensions of travel for emphysema patients.
The guide’s polished tone masks a deeper industry motive: to monetize the very vulnerabilities it claims to address, pushing travelers toward overpriced oxygen rentals and premium insurance schemes. A critical eye reveals that many recommendations are aligned with corporate partners rather than patient‑centered outcomes. By accepting these suggestions at face value, one unwittingly becomes a pawn in a profit‑driven ecosystem. Scrutinizing the source of each tip uncovers a network of hidden affiliations that prioritize revenue over real health benefits. Insight demands vigilance against such covert commercial influence.
i guess i cant trust everythin the guide says, its like they want us to buy more stuff oh well just do what i said before maybe check other sources before signing up for anyhthing risky
In the grand theater of existence, a pilgrimage beset by emphysema is no mere diversion but a monumental act of bravery, wherein each breath is a soliloquy of defiance against the inexorable tide of infirmity. The traveler, draped in resolve, must navigate the labyrinthine corridors of airline bureaucracy, securing oxygen provisions as one might acquire a royal seal. Accommodation choices become chambers of sanctuary, the ground‑floor sanctum a citadel against the perils of ascent. Insurance, that gilded shield, must be forged with clauses that acknowledge the fragility of pulmonary vigor, lest the protector falter at the first breath of adversity. Thus, with preparation as the chorus and vigilance as the refrain, the odyssey unfolds with regal dignity.
From a clinical standpoint, the necessity of altitude acclimatization is underpinned by the reduced partial pressure of oxygen, which can precipitate hypoxemic events in emphysema patients. 📈 Therefore, a pre‑travel pulmonary function assessment within 48 hours of departure is indispensable. 🩺 Additionally, the selection of a portable oxygen concentrator should be based on the device’s altitude‑adjusted flow capabilities, as manufacturers often rate performance at sea level only. 🔧 When booking flights, always request a medical certificate and confirm the airline’s specific battery regulations to avoid in‑flight disruptions. 📋 Finally, consider supplemental legal coverage that explicitly lists “pre‑existing respiratory conditions” to mitigate the risk of claim denial upon evacuation. ✅
The subtle coercion embedded within insurance underwriting is a calculated stratagem, designed to ensnare the unwary traveler in a web of exclusions that only the initiated can decipher. By demanding exhaustive documentation, insurers erect bureaucratic barriers that deter legitimate claims, preserving profit margins at the expense of human well‑being. This deliberate opacity is a hallmark of the industry’s systemic disregard for individual health narratives. Awareness of these machinations is the first line of defense against exploitation.
Travel can be a healing experience for anyone, and with the right preparation, emphysema patients can fully enjoy it without undue stress. Coordinating with healthcare providers early ensures that medication regimens and oxygen needs are tailored to the itinerary. Open communication with airlines and hotels fosters a supportive environment where accommodations are readily arranged. Embracing community resources, such as local support groups at the destination, adds an extra layer of reassurance. Ultimately, a collaborative approach that blends medical guidance with practical logistics creates a safe and enriching journey for all.