Contact dermatitis is a skin inflammation caused by direct exposure to irritants or allergens, marked by redness, itching, and occasional blistering. It touches millions worldwide and often forces people to hide their skin, which can ripple into emotional distress.
Why the Skin‑Mind Connection Matters
Our skin is the body’s largest organ and a constant visual cue to the outside world. When it’s inflamed, the brain receives pain signals, and the social brain picks up on perceived judgment. Studies from the New Zealand Dermatology Society (2023) show that 42% of people with chronic contact dermatitis report moderate to severe anxiety. The link between visible skin disease and self‑esteem is a two‑way street: the more a person worries about appearance, the more they notice symptoms, creating a feedback loop.
Key Players: From Irritants to Emotions
Understanding the main actors helps break the cycle.
- Irritant contact dermatitis results from direct chemical damage (e.g., detergents, solvents)
- Allergic contact dermatitis is an immune‑mediated reaction to allergens such as nickel or fragrance mixes
- Anxiety is a heightened state of worry that can intensify itch perception
- Depression often co‑occurs with chronic skin conditions, reducing motivation for self‑care
- Quality of life measures overall well‑being, frequently lowered in dermatitis patients
- Psychodermatology is the interdisciplinary field linking skin disorders with mental health
- Dermatology care includes topical therapies, patch testing, and counseling
Comparing Irritant and Allergic Forms
| Attribute | Irritant Contact Dermatitis | Allergic Contact Dermatitis |
|---|---|---|
| Primary cause | Direct chemical damage | Immune‑mediated allergy |
| Latency | Immediate (minutes to hours) | Delayed (24‑72 hrs) |
| Typical triggers | Detergents, solvents, acids | Nickel, fragrance mix, latex |
| Prevalence | ≈ 60% of cases | ≈ 40% of cases |
| Psychological impact | Often linked to occupational stress | Higher association with anxiety due to unpredictability |
Both types can spark the same mental health fallout, but allergic reactions tend to feel less controllable, amplifying worry.
How Contact Dermatitis Triggers Psychological Strain
Three pathways dominate:
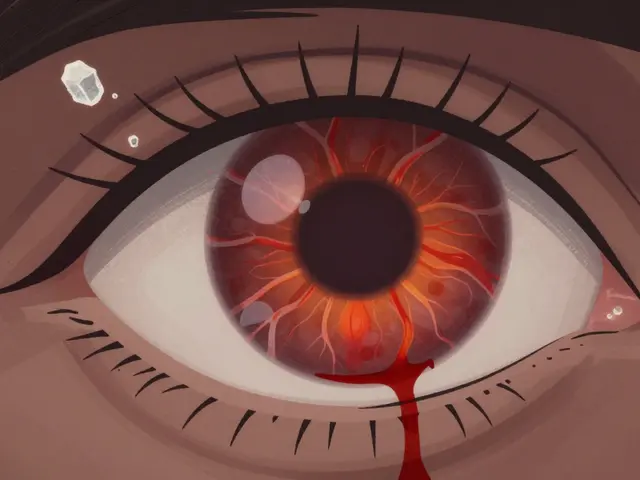
- Physical discomfort: Persistent itch (pruritus) releases histamine, which also stimulates brain regions tied to anxiety.
- Social visibility: Visible lesions can lead to stigma. A 2022 survey of 1,200 New Zealand workers found that 27% avoided social gatherings because of skin flare‑ups.
- Treatment burden: Daily creams, avoidance routines, and medical appointments add chronic stress, eroding coping reserves.
When these factors pile up, the risk of clinical depression rises. A longitudinal study from the University of Auckland (2021) reported a 1.8‑fold increase in depressive scores among participants with severe dermatitis over a 5‑year span.

Assessment Tools: Measuring the Dual Impact
Clinicians now use combined scales to capture both skin severity and mental health:
- SCORAD Quantifies eczema severity, also applicable to contact dermatitis
- DLQI (Dermatology Life Quality Index) Scores the impact on daily activities and emotional state
- HADS (Hospital Anxiety and Depression Scale) Screens for anxiety and depression in dermatology patients
Using these together gives a fuller picture; a high SCORAD with a low HADS suggests physical disease dominates, whereas the opposite flags a mental‑health priority.
Practical Strategies to Protect Mental Well‑Being
Below are evidence‑based steps that patients and clinicians can adopt.
1. Identify and Eliminate Triggers
Patch testing remains the gold standard for pinpointing allergens. Once identified, replace nickel‑bearing jewelry or switch to fragrance‑free cleaners. Occupational health services can supply safer alternatives for workers exposed to solvents.
2. Adopt Skin‑Soothing Regimens
Barrier creams with ceramides reduce irritant damage by up to 30% (New Zealand Dermatology Journal, 2023). Pair creams with lukewarm showers and gentle cleansers to limit barrier disruption.
3. Incorporate Mind‑Body Techniques
Mindfulness‑based stress reduction (MBSR) cuts itch intensity by an average of 15 points on a 100‑point visual analogue scale (randomized trial, 2022). Simple breathing exercises before bedtime can also lower nocturnal flare‑ups.
4. Seek Professional Mental Health Support
Cognitive‑behavioral therapy (CBT) tailored to chronic illness improves both DLQI and HADS scores. Many public health clinics in Hamilton now offer integrated dermatology‑psychology appointments.
5. Build a Support Network
Online forums such as the New Zealand Skin Health Community provide peer validation. Sharing stories reduces isolation and often surfaces practical tips about product substitutions.
6. Monitor Progress Regularly
Track symptoms in a diary, noting flare‑up triggers, emotional state, and treatment adherence. Apps designed for eczema management can be repurposed for contact dermatitis, helping both patient and doctor spot patterns.
Related Concepts Worth Exploring
Understanding the broader ecosystem helps keep the conversation going.
- Psychodermatology connects skin disorders with mental health, offering a framework for interdisciplinary care.
- Chronic skin disease burden looks at the cumulative economic and social costs of long‑term conditions.
- Occupational dermatitis focuses on workplace exposures and preventative regulations.
- Mind‑body connection explores how stress hormones influence skin inflammation.
Readers interested in any of these topics will find deeper dives in our sister articles on stress‑related skin flare‑ups, occupational health guidelines, and holistic dermatology approaches.
Next Steps for Readers
1. Take a quick online DLQI questionnaire to gauge your current quality of life. 2. Book a patch test if you suspect an allergic trigger. 3. Try a 7‑day mindfulness log and note any change in itch severity. 4. Reach out to a local support group - sharing is often the first step toward healing.

Frequently Asked Questions
Can contact dermatitis lead to depression?
Yes. Chronic itch and visible lesions can erode self‑esteem and limit social activities, which are known risk factors for depression. Studies in New Zealand show a 1.8‑fold increase in depressive symptoms among patients with severe, long‑standing dermatitis.
What’s the difference between irritant and allergic contact dermatitis?
Irritant dermatitis results from direct chemical damage and appears quickly after exposure. Allergic dermatitis is an immune reaction that takes 24‑72hours to develop and requires prior sensitisation to the allergen. Both cause redness and itching, but the allergic form is often more unpredictable.
How can I tell if my anxiety is making my dermatitis worse?
If you notice that flare‑ups occur during stressful periods, or if itch intensifies when you’re worried, anxiety may be amplifying your symptoms. Keeping a diary that logs mood, stress levels, and skin changes can reveal the pattern.
Are there any over‑the‑counter products that help both skin and mind?
Barrier creams containing ceramides support the skin’s protective layer, while topical menthol can provide a cooling sensation that temporarily reduces itch‑related anxiety. Pairing these with a daily mindfulness app creates a dual approach.
When should I see a mental‑health professional?
If you score 8 or higher on the Hospital Anxiety and Depression Scale (HADS) or if skin symptoms are interfering with work, relationships, or sleep, it’s time to get professional help. Integrated dermatology‑psychology clinics can address both issues in one visit.


Look, I'm not buying the idea that every rash needs a therapist-most people just need better soap and less stress about what others think. The article throws around fancy terms while ignoring the simple fact that good barrier care solves the bulk of irritant cases.
yeah, i get u, but a pinch of mental health support isn’t a bad idea – a quick chat with a counsellor can actually help you stick to your skin routine, y’know? plus, those mindfulness apps are pretty chill for keeping the itch anxiety low.
You’ve got this keep logging your flares and try those ceramide creams they really help
The interrelationship between cutaneous inflammation and psychological well‑being has been the subject of intensive investigation within the field of psychodermatology for several decades.
Empirical evidence consistently demonstrates that patients with chronic contact dermatitis experience a measurable increase in anxiety scores relative to healthy controls.
This phenomenon can be attributed, in part, to the persistent nociceptive input generated by pruritic lesions, which activates central pathways involved in stress modulation.
Moreover, the conspicuous nature of visible dermatoses precipitates a heightened self‑consciousness that may exacerbate social withdrawal.
Consequently, a bidirectional feedback loop emerges wherein psychological distress amplifies perceived itch intensity, which in turn intensifies the somatic manifestation of the disease.
From an occupational perspective, irritant contact dermatitis frequently afflicts individuals employed in industries with repetitive exposure to chemicals, thereby intertwining concerns of job security with health anxieties.
Allergic contact dermatitis, while less prevalent, introduces an element of unpredictability that can further destabilise a patient’s sense of control.
Clinical assessment tools such as the Dermatology Life Quality Index and the Hospital Anxiety and Depression Scale provide quantifiable metrics that facilitate the integration of dermatologic and psychiatric care.
Recent longitudinal studies have revealed that early implementation of cognitive‑behavioral interventions can attenuate the escalation of depressive symptomatology in this patient cohort.
In parallel, advances in barrier repair technology, including ceramide‑enriched emollients, have shown efficacy in reducing transepidermal water loss and consequently diminishing the neurogenic component of itch.
It is imperative that healthcare providers adopt a multidisciplinary approach, coordinating dermatologists, psychologists, and occupational health specialists to address the multifactorial nature of the condition.
Patient education remains a cornerstone of management, empowering individuals to identify triggers, adhere to treatment regimens, and employ stress‑reduction techniques such as mindfulness‑based stress reduction.
Furthermore, community support networks, both in‑person and digital, have been documented to mitigate feelings of isolation and promote coping strategies.
Economic analyses suggest that comprehensive care models not only improve quality of life but also reduce long‑term healthcare expenditures associated with chronic disease management.
Future research should aim to elucidate the molecular mechanisms linking cytokine release to affective disorders, thereby opening avenues for targeted pharmacologic therapies.
In summary, the convergence of dermatologic and psychiatric expertise offers the most promising pathway toward alleviating the dual burden imposed by contact dermatitis.
Oh great, another 16‑sentence dissertation – next you’ll prescribe meditation for my broken toe 😏
Isn't it wild how a tiny patch of red can feel like the whole world is watching you? We chase after ointments like they're holy relics, yet the real battle is inside our heads – a storm of doubt that swirls whenever the skin cries out. It’s a tragic comedy, and we’re the unwilling actors.
Applying a barrier cream twice daily can significantly reduce irritant dermatitis symptoms.
Indeed, consistent barrier protection not only mitigates cutaneous inflammation but also contributes to psychological reassurance, as patients perceive greater control over their condition.
I appreciate the practical tips shared here; integrating them gradually can help anyone manage both the physical and emotional aspects of dermatitis without feeling overwhelmed.
When we view skin health through a holistic lens, the synergy between routine care and mindful self‑compassion becomes evident, fostering resilience that extends beyond the epidermis.