Hormone Balance Calculator
Progesterone & Estrogen Balance Calculator
Understand how your hormone levels relate to uterine fibroid risk based on your test results.
Important Note: This calculator provides general information only. Consult your healthcare provider for personalized medical advice regarding hormone levels and fibroid management.
Ever wonder why some women develop uterine fibroids even when they’re careful about diet and exercise? The missing piece often comes down to hormones-specifically, a shortage of progesterone. Below we break down what progesterone does, how its deficiency fuels fibroid growth, and what you can do to bring balance back.
Understanding Progesterone and Its Role
Progesterone is a steroid hormone produced mainly by the ovaries after ovulation, essential for preparing the uterine lining for pregnancy and moderating the effects of estrogen. In a healthy menstrual cycle, progesterone rises after the egg is released, signaling the endometrium to become secretory. It also tells the uterine muscle (myometrium) to stay calm, preventing excessive tissue growth.
When progesterone levels dip, estrogen can act unchecked, leading to a kind of hormonal “wild west” in the uterus.
What Are Uterine Fibroids?
Uterine fibroids are non‑cancerous tumors that arise from the smooth muscle cells (myometrial cells) and connective tissue of the uterus. They’re common-affecting up to 70% of women by age 50-but many never notice them. Symptoms appear when fibroids grow large enough to press on surrounding structures, causing heavy bleeding, pelvic pain, or pressure on the bladder.
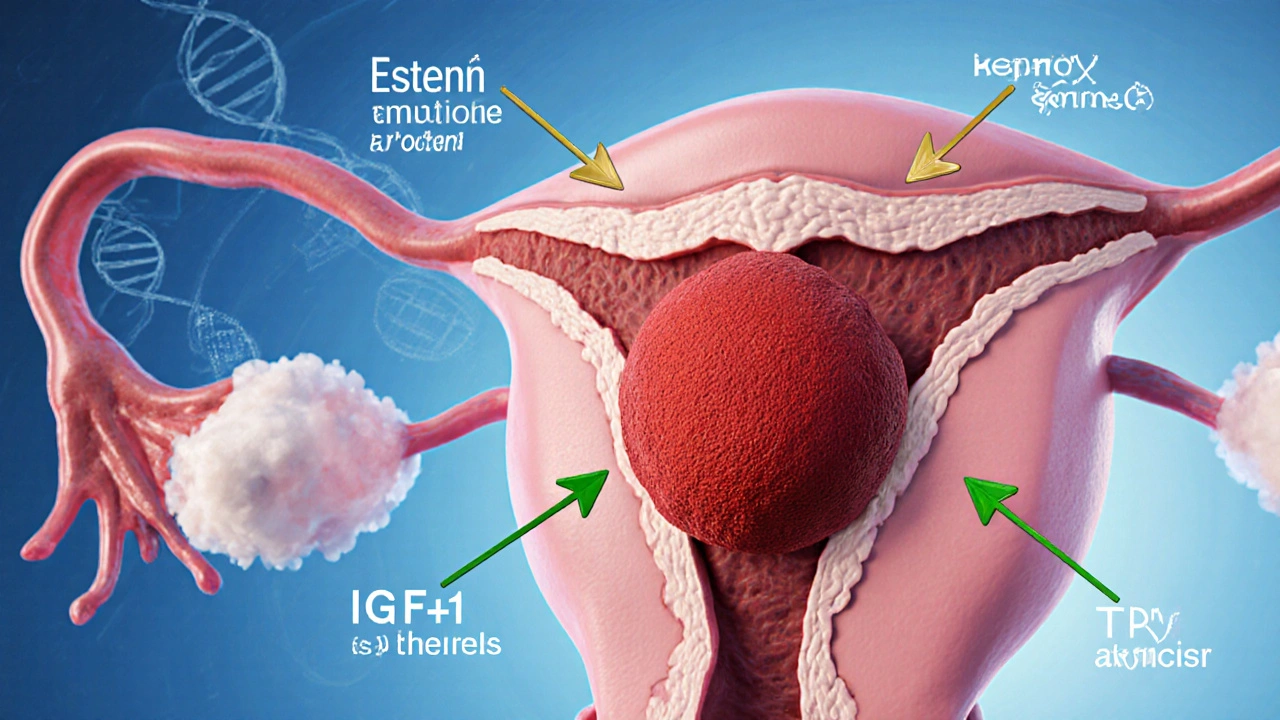
How Low Progesterone Fuels Fibroid Growth
Fibroids thrive on a hormonal environment where estrogen dominates and progesterone cannot counterbalance it. Here’s the chain reaction:
- Estrogen spikes: Without enough progesterone, estrogen continues to stimulate cell proliferation in the myometrium.
- Growth‑factor surge: Low progesterone raises levels of insulin‑like growth factor (IGF‑1) and transforming growth factor‑beta (TGF‑β), both of which encourage fibroid cells to multiply.
- Extracellular matrix buildup: Progesterone normally regulates collagen turnover. A deficit leads to excess collagen, making fibroids denser and harder to shrink.
- Impaired apoptosis: Progesterone triggers programmed cell death in abnormal myometrial cells. When it’s missing, those cells linger and form tumors.
In short, low progesterone removes the “brakes” that keep estrogen‑driven growth in check, allowing fibroids to expand.
Spotting the Signs of Hormonal Imbalance
Hormonal shifts don’t always announce themselves with dramatic symptoms. Look for these subtle clues that progesterone might be low:
- Irregular periods-especially a shortened luteal phase (the time between ovulation and menstruation).
- Spotting or heavier bleeding than usual.
- Premenstrual mood swings that feel out of proportion.
- Difficulty getting pregnant or early miscarriage.
- Persistent lower‑back or pelvic discomfort that isn’t linked to other conditions.
If you notice several of these, it’s worth checking your hormone profile.
Testing Progesterone Levels
A reliable way to confirm a deficiency is a serum progesterone test taken about a week after ovulation (day21 of a typical 28‑day cycle). Normal luteal‑phase ranges are roughly 5-20ng/mL, though exact cut‑offs can vary by lab.
For women with irregular cycles, doctors may use a basal body temperature chart or ovulation predictor kits to pinpoint ovulation before drawing blood. Saliva or urinary progesterone tests exist but are less precise for clinical decision‑making.
Besides progesterone, a comprehensive hormone panel often includes:
- Estrogen (estradiol) - to see the estrogen‑progesterone ratio.
- Testosterone - high levels can co‑stimulate fibroid growth.
- Progesterone‑binding globulin - informs how much hormone is free to act.
Interpretation should be done by a practitioner familiar with reproductive endocrinology.

Managing Low Progesterone to Control Fibroids
Once a shortfall is confirmed, several medical routes can help rebalance hormones and shrink fibroids:
- Progestin therapy: Oral micronized progesterone or a vaginal gel supplies the missing hormone, often reducing heavy bleeding.
- GnRH agonists: These temporarily shut down ovarian hormone production, causing fibroids to shrink, but they also lower progesterone, so they’re usually combined with add‑back progestin.
- Aromatase inhibitors: By limiting estrogen synthesis, they indirectly ease the pressure on progesterone.
- Uterine artery embolization (UAE): A minimally invasive procedure that cuts off blood flow to fibroids, leading to shrinkage. Hormone levels are monitored before and after to gauge recurrence risk.
- Myomectomy: Surgical removal of fibroids, often recommended when size or location causes severe symptoms. Post‑op hormone therapy may prevent regrowth.
Choosing the right path depends on fibroid size, location, desire for future pregnancy, and how severe the hormonal imbalance is.
Lifestyle Moves that Support Hormone Balance
Medical treatment works best alongside everyday habits that nurture progesterone production:
- Eat progesterone‑boosting foods: VitaminB6‑rich choices like chickpeas, banana, and salmon help the corpus luteum make more hormone.
- Maintain steady blood sugar: Spikes in insulin can increase androgen production, which in turn can suppress progesterone. Aim for balanced meals with protein, fiber, and healthy fats.
- Manage stress: High cortisol blocks progesterone synthesis. Practices such as mindfulness, yoga, or simple breathing exercises can keep cortisol in check.
- Get 7‑9 hours of sleep: Sleep deprivation disrupts the hypothalamic‑pituitary‑ovarian axis, lowering luteal‑phase progesterone.
- Exercise intelligently: Moderate aerobic activity improves circulation to the ovaries. Over‑training, however, can push hormones the other way, so aim for 150 minutes of moderate activity per week.
- Consider herbal allies: Vitex (chaste tree berry) has been shown in small trials to raise luteal‑phase progesterone by up to 30% when taken consistently for three months.
These steps won’t replace a doctor’s advice, but they create a hormonal environment that makes fibroid growth less likely.
Frequently Asked Questions
Can low progesterone cause fibroids to appear for the first time?
Yes. While genetics set the stage, a sustained progesterone deficit removes the hormonal brake, allowing estrogen‑driven cells to form new fibroids or enlarge existing ones.
Do birth control pills help with fibroids linked to low progesterone?
Combined oral contraceptives supply both estrogen and progestin, which can stabilize the hormone ratio and often lessen bleeding. However, some formulations with higher estrogen may still promote growth, so a low‑dose progestin‑only pill is often a better choice for fibroid patients.
Is progesterone therapy safe if I want to get pregnant?
Micronized progesterone is considered safe in the luteal phase for women trying to conceive because it mimics the body’s natural hormone. It can actually improve implantation rates when the luteal‑phase length is short.
How long does it take for fibroids to shrink after fixing progesterone levels?
Clinical studies show a modest reduction (10‑20% in volume) after 3‑6 months of consistent progestin therapy, especially for smaller (<5cm) fibroids. Larger lesions often need additional interventions.
Can diet alone raise my progesterone enough to affect fibroids?
Diet can boost the building blocks, but profound hormonal shifts typically require a medical component. Think of diet as a supportive layer rather than a sole cure.


Your exposition on hormonal dynamics scarcely scratches the surface of the intricate endocrinological symphony governing uterine pathophysiology.
Thank you for compiling such a thorough overview. Recognizing progesterone’s role can empower women to seek targeted testing. It’s especially valuable to highlight lifestyle measures alongside medical options. I encourage readers to discuss these strategies with a qualified provider.
Stop acting like this is some new revelation progesterone has been studied for decades.
People need to stop blaming diets and start looking at hormone imbalance it’s basic biology.
Oh sure, because the universe is just waiting for us to “balance” hormones before we can have a child. The drama of low progesterone being blamed for every fibroid is a convenient narrative for those who avoid confronting genetic predisposition.
I cant believe how many women are left in the dark about this… it’s like the medical community is whisperin’ secrets while we suffer the consequences.
What they don’t tell you is that the pharma giants have a vested interest in keeping progesterone “deficiency” a hot topic – it drives sales of endless supplements and hormone‑replacement drugs. Wake up, folks, the agenda is crystal clear.
Indeed, the interplay between luteal‑phase progesterone secretion and estrogenic proliferative signaling constitutes a crucial axis; when this axis is perturbed, the downstream activation of growth‑factor pathways-such as IGF‑1 and TGF‑β-facilitates myometrial hyperplasia, ultimately manifesting as fibroids.
Great summary, very helpful.
Well, if we’re to dissect the hormonal ballet that supposedly orchestrates fibroid genesis, we might as well bring out the lab coats and chalkboards for a full symposium. First, the article correctly points out that progesterone acts as a biological brake, but it conveniently glosses over the fact that estrogen’s role is not merely a reckless speedster-it also engages in nuanced receptor‑mediated actions that can be both proliferative and anti‑proliferative depending on the isoform. Second, the notion that low progesterone “removes the brakes” oversimplifies a cascade involving aromatase activity, local tissue conversion, and paracrine loops that are still being mapped. Third, lifestyle factors such as insulin resistance and chronic inflammation are mentioned in passing, yet they have substantial evidence linking them to altered steroidogenesis. Fourth, the piece mentions Vitex as a herbal ally, but the clinical trials are scant and often plagued by methodological flaws. Fifth, the recommendation to monitor luteal‑phase progesterone on day 21 assumes a textbook 28‑day cycle, ignoring the reality of anovulatory patterns in many women. Sixth, while progestin therapy can reduce bleeding, it does not universally shrink fibroids, and in some cases may even exacerbate them. Seventh, the risk calculator at the top of the article appears to use a simplistic ratio without accounting for age, BMI, or genetic predisposition-variables that dramatically shift risk profiles. Eighth, the article’s warning that “low progesterone contributes to fibroid growth” is technically correct but might mislead readers into thinking that hormone replacement is a panacea. Ninth, the emphasis on “dietary progesterone‑boosting foods” borders on pseudoscience, as the conversion of dietary precursors to active hormone is tightly regulated. Tenth, the discussion of GnRH agonists mentions add‑back therapy but fails to elaborate on the potential for hypo‑estrogenic side effects. Eleventh, the brief mention of uterine artery embolization neglects the fact that post‑procedure hormonal shifts can precipitate recurrence. Twelfth, the alternative of myomectomy is described without addressing the substantial scar tissue that can itself alter hormonal microenvironments. Thirteenth, the article’s tone, while earnest, sometimes drifts into alarmist language, which can heighten anxiety rather than empower. Fourteenth, the overall lack of citation of primary literature leaves the reader guessing about the evidentiary foundation. Fifteenth, despite all these caveats, the piece does a commendable job of raising awareness, which is arguably its primary mission. In short, while the hormone‑centric lens is valuable, a more holistic, evidence‑based framework would serve patients better.
Hormones are complicated, but the fact that the industry pushes “progesterone boosters” while hiding the real data is infuriating 😡🧬. Keep questioning the source of your supplements!
yeah right another “miracle” herb that will fix everything lol.
Excellent breakdown! 😊 Remember, if you suspect a hormone imbalance, a simple blood test with your OB‑GYN can clarify things. Don't hesitate to ask about progesterone support options.
Spot on! The interplay of IGF‑1 and TGF‑β in the myometrium is exactly why we need to look beyond just “low progesterone” and address the whole signaling network.
Honestly, fibroids are mostly genetic – hormone talk is just a convenient excuse.
i think the whole talk about balance is kinda like chasing a moving target – kinda deep, kinda silly.