Many people don’t realize that their eye drops or pills can lose effectiveness-or even become harmful-if stored the wrong way. If your medication says "protect from light" on the label, it’s not just a suggestion. It’s a requirement. Exposure to sunlight or even bright indoor lighting can break down the active ingredients, turning a life-saving treatment into something useless-or worse. This isn’t theoretical. Studies show some eye drops lose up to 40% of their potency after just seven days in a clear bottle. And it’s not just eye drops. Antibiotics, hormone treatments, and even vitamin D drops can degrade when exposed to light. The result? Medications that don’t work as they should. That’s dangerous.
Why Light Destroys Medications
Light, especially UV rays, triggers chemical reactions in certain drugs. These reactions change the structure of the molecules, making them less effective or creating harmful byproducts. For example, tetracycline antibiotics can turn toxic when exposed to sunlight. Nitroglycerin, used for chest pain, can lose its ability to open blood vessels. Eye drops are especially vulnerable because they’re liquid and often stored in small, clear containers that let in plenty of light. A 2021 study by Alcon found that eye drops stored in clear plastic lost 35% of their strength in just 14 days. The same drops in amber bottles stayed stable for the full shelf life.The U.S. Pharmacopeia (USP) now requires that light-sensitive medications be packaged in containers that block wavelengths below 470 nanometers. That’s why you see brown or amber bottles. These aren’t just colored glass-they’re engineered to block the exact part of the light spectrum that damages drugs. Amber glass blocks 98% of UV light. High-quality opaque plastic blocks about 85%. That difference matters.
What Medications Need Protection?
Not all medications are light-sensitive, but many common ones are. Here’s a quick list of types that require special storage:- Eye drops: Especially glaucoma meds like latanoprost, timolol, and bimatoprost. These are water-based and degrade fast in light.
- Antibiotics: Tetracycline, doxycycline, and ciprofloxacin. Discoloration (yellowing or browning) is a red flag.
- Hormone treatments: Birth control pills, thyroid meds, and some chemotherapy drugs.
- Biologics: Insulin, certain injectables for arthritis or autoimmune diseases. These are fragile and need both cold and dark storage.
- Vitamin D supplements: Liquid forms can turn cloudy or oily when exposed to light.
- Anti-seizure meds: Phenobarbital and carbamazepine.
If your medication comes in a clear bottle, it’s likely not light-sensitive. But if it’s in amber, brown, or opaque plastic, treat it like a time bomb if you leave it on the counter. Check the label. If it says "protect from light," "store in original container," or "keep in dark place," follow those instructions exactly.
Where to Store Them
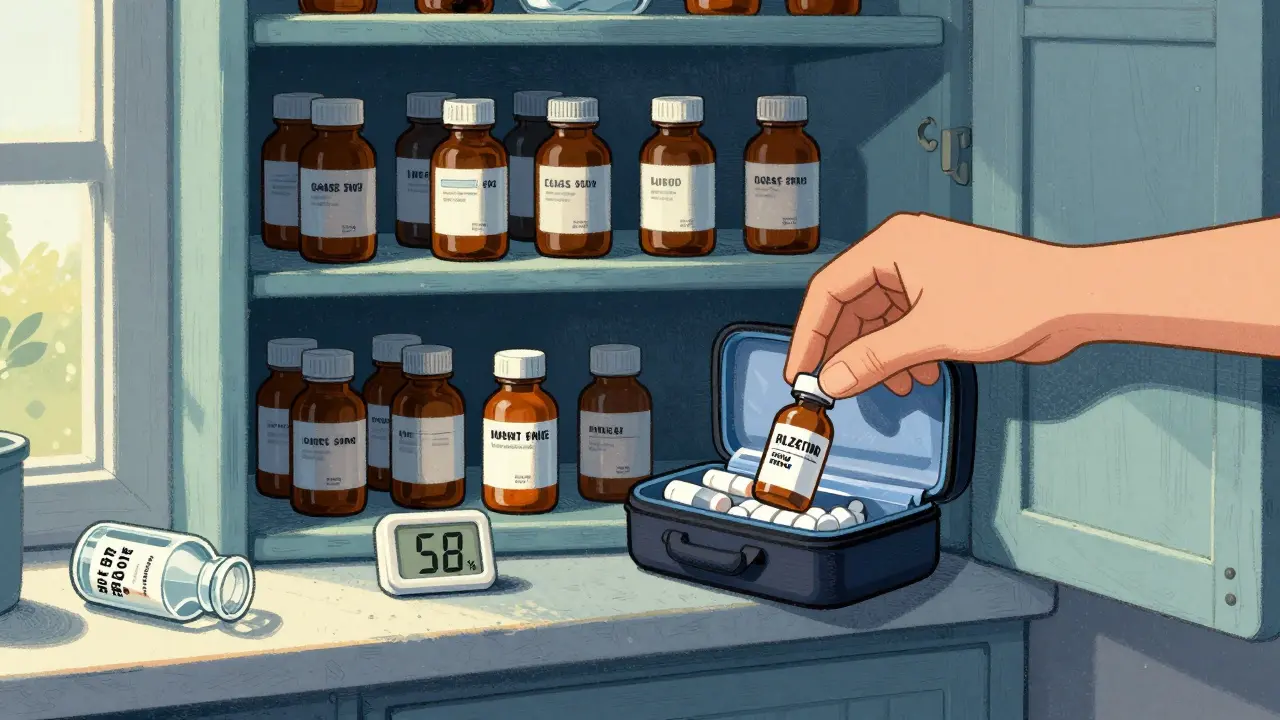
Your bathroom cabinet is the worst place. Heat, steam, and light from the overhead bulb all attack your meds. The same goes for windowsills, nightstands near lamps, or medicine boxes on top of the fridge. Instead, pick a cool, dry spot away from direct light.The best option? A kitchen cabinet, away from the stove and sink. These areas stay consistently cool and rarely get direct sunlight. A drawer in a bedroom dresser works too. The key is consistency: no big temperature swings, no humidity, and no light. The ideal temperature range for most medications is between 59°F and 77°F (15°C-25°C). If your home gets hotter than 86°F in summer, you need a backup plan.
For eye drops, once opened, most can be stored at room temperature for up to 6 weeks-but only if they’re in their original amber bottle. Never transfer them to a clear container, even if it’s labeled "for eye drops." That’s one of the most common mistakes. A 2023 American Academy of Ophthalmology report found that 18% of eye treatment failures were linked to patients pouring drops into new, non-protective bottles.
Special Cases: Insulin and Biologics
Insulin and other biologics need both refrigeration and light protection. Unopened vials should stay in the fridge at 36°F-46°F (2°C-8°C). Once opened, they can be kept at room temperature for up to 28 days-but still away from light. If you travel, use an insulated cooler with a UV-blocking lining. These cost around $25-$50 and keep meds stable for 8-12 hours. Some newer models even have temperature sensors that alert you via Bluetooth if things get too warm.Don’t leave insulin on the dashboard of your car. Don’t put it in a purse that sits in direct sunlight. A 2022 FDA report noted that 327 adverse events that year were linked to improper storage of injectables, with light exposure cited in over 40% of cases.
Storage Options Compared
| Option | Light Protection | Temperature Stability | Cost | Convenience |
|---|---|---|---|---|
| Amber glass bottle (original) | 98% | Good | $0.08-$0.20/unit | High |
| Opaque plastic bottle | 85% | Good | $0.15-$0.35/unit | High |
| Aluminum foil pouch | 100% | Poor (requires removal) | $0.10-$0.25/unit | Low |
| UV-blocking storage box | 95% | Good | $19.99-$59.99 | Medium |
| Insulated travel case with UV lining | 90% | Excellent | $25-$60 | Medium |
Amber glass is the gold standard. It’s durable, reusable, and blocks nearly all harmful light. Opaque plastic is cheaper and lighter but slightly less effective. Foil pouches block 100% of light, but you have to unwrap your meds every time you use them. That’s why 32% of patients stop using them properly. Storage boxes are great for families with multiple light-sensitive meds. They’re like a mini-fridge for pills-dark, cool, and centralized.
Signs Your Medication Has Degraded
You don’t need a lab to tell if your meds are bad. Look for these signs:- Discoloration: Creams or liquids that turn yellow, brown, or cloudy. Tretinoin cream turning from white to yellow? Pitch it.
- Change in texture: Pills that crumble, ointments that separate, or eye drops that look oily or stringy.
- Strange smell: Aspirin that smells like vinegar? It’s broken down. Don’t take it.
- Loss of effect: If your glaucoma drops aren’t lowering eye pressure like they used to, or your antibiotic isn’t clearing an infection, light exposure might be why.
One Reddit user, "MedTechRN," threw out $120 worth of compounded tretinoin cream after it turned yellow in a bathroom cabinet. "I didn’t know light could do that," they wrote. "Now I keep everything in a drawer."
Travel Tips
Traveling? Pack your meds in a small insulated bag with UV-blocking lining. Keep them in your carry-on, not checked luggage. Temperatures in airplane cargo can drop below freezing or soar above 100°F. Don’t leave your eye drops in a hot car. If you’re flying, ask your pharmacist for a travel-sized amber bottle. Many pharmacies will transfer your meds into a smaller, compliant container for free.
What Not to Do
Avoid these common mistakes:- Don’t transfer meds to new containers. Even if it’s "clean" or "clear." The original packaging was designed for a reason.
- Don’t store near windows, sinks, or appliances. Heat and light come from all directions.
- Don’t ignore expiration dates. Even if stored perfectly, light-sensitive meds degrade faster after opening. Most eye drops last 4-6 weeks after opening. Write the opening date on the bottle.
- Don’t assume "cool" means "dark." A fridge is cool, but if it’s in a clear plastic bag on the shelf, it’s still exposed to light.
When to Throw It Out
If you’re unsure, throw it out. It’s not worth the risk. The FDA’s MedWatch program recorded over 1,800 adverse events in 2022 linked to improper storage. Most involved people who kept meds "just in case" even after they looked off. That’s how you end up with a failed treatment-or worse.Here’s a simple rule: If it looks, smells, or feels wrong, toss it. Replace it. Your health isn’t worth gambling on.
Final Tips
- Check labels every time you refill a prescription. New formulations may have different storage needs.
- Use a small hygrometer to monitor humidity in your storage area. Ideal is below 60%.
- Keep meds out of reach of kids and pets. Amber bottles aren’t childproof.
- Ask your pharmacist: "Is this medication light-sensitive?" They can check the USP database in seconds.
Proper storage isn’t complicated. It’s just consistent. Put your meds where it’s dark, cool, and dry. Use the original container. Don’t move them. And if you’re ever in doubt-throw it out and get a new one.
Can I store eye drops in the fridge?
Yes, but only if the label says so. Most eye drops can be stored at room temperature after opening (between 40°F-77°F). Refrigeration can make them feel uncomfortable when applied. However, if your eye drops are labeled "refrigerate," keep them cold. Just make sure they’re still in their original amber bottle. Never freeze eye drops-this can damage the formulation.
What if I left my eye drops in the sun for a day?
If your eye drops were in a clear bottle and left in direct sunlight for more than a few hours, assume they’ve degraded. Even if they look fine, their potency may have dropped by 20-40%. Don’t risk using them. Discard them and get a new prescription. For amber bottles, brief exposure is less risky-but still not ideal. Always store them in a dark place, even if they’re in the right container.
Are all eye drops light-sensitive?
No, but most are. Antibiotics, glaucoma meds, anti-inflammatory drops, and steroid eye solutions are typically light-sensitive. Artificial tears without preservatives usually aren’t. Always check the label. If it says "protect from light," "store in original container," or has an amber bottle, treat it as sensitive. If the bottle is clear and the label doesn’t mention light, it’s likely safe at room temperature.
Can I use a dark drawer instead of an amber bottle?
Only if the medication is already in an amber or opaque container. Putting a clear bottle in a dark drawer doesn’t fully protect it. Light can still penetrate the plastic or glass over time, especially if the drawer is opened often. The container itself must block UV light-not just the environment. That’s why manufacturers use amber glass or UV-blocking plastic: it protects from all angles, even when you’re not thinking about it.
How do I know if my medication is light-sensitive?
Check the packaging. Look for phrases like "protect from light," "store in original container," or "keep away from direct sunlight." The bottle color is also a clue: amber, brown, or opaque plastic means yes. Clear bottles usually mean no. You can also ask your pharmacist or check the FDA’s online drug database. If the medication is listed as requiring photostability testing, it’s light-sensitive. When in doubt, assume it is.




Okay, so let me get this straight - the FDA and USP are basically saying that your eye drops are a ticking time bomb if you don’t store them like nuclear waste? And we’re supposed to trust that amber bottles are 98% effective? What about the fact that most of these bottles are made in China or India with recycled plastic that’s been UV-bleached a hundred times? I’ve seen the manufacturing logs. The dye they use in amber glass? It’s not even consistent. Some batches leak 12% UV. And don’t even get me started on how pharmacies refill these things in uncontrolled environments. I worked in a compounding lab. We had a guy who’d rinse bottles with tap water and dry them on the windowsill. Yeah. Windowsill. I’m not saying this is conspiracy, I’m saying it’s negligence wrapped in a pretty brown bottle. You think your glaucoma drops are working? They’re probably 30% degraded. You’re just not blind enough to notice yet.