Why Metformin and Contrast Dye Are a Concern
Every year, millions of people with type 2 diabetes get imaging scans using contrast dye-CT scans, angiograms, or other procedures that need iodinated contrast to highlight blood vessels or organs. If you’re on metformin, you’ve probably heard the warning: stop your metformin before the scan. But is that still necessary? The answer isn’t as simple as it used to be.
Back in the 1990s, doctors were terrified of metformin. It was linked to lactic acidosis-a rare but deadly condition where lactic acid builds up in the blood, making it too acidic. The fear was that contrast dye could damage the kidneys, which would then fail to clear metformin from the body. The buildup could trigger lactic acidosis. So the rule was simple: stop metformin before any scan, wait 48 hours, then restart.
But here’s the truth: metformin-induced lactic acidosis is extremely rare. Studies show fewer than 10 cases per 100,000 patients per year. And most of those cases happened in people who were already very sick-severely dehydrated, in heart failure, or with advanced kidney disease. Contrast dye alone? It doesn’t cause lactic acidosis in healthy kidneys.
How Metformin Works (and Why Kidneys Matter)
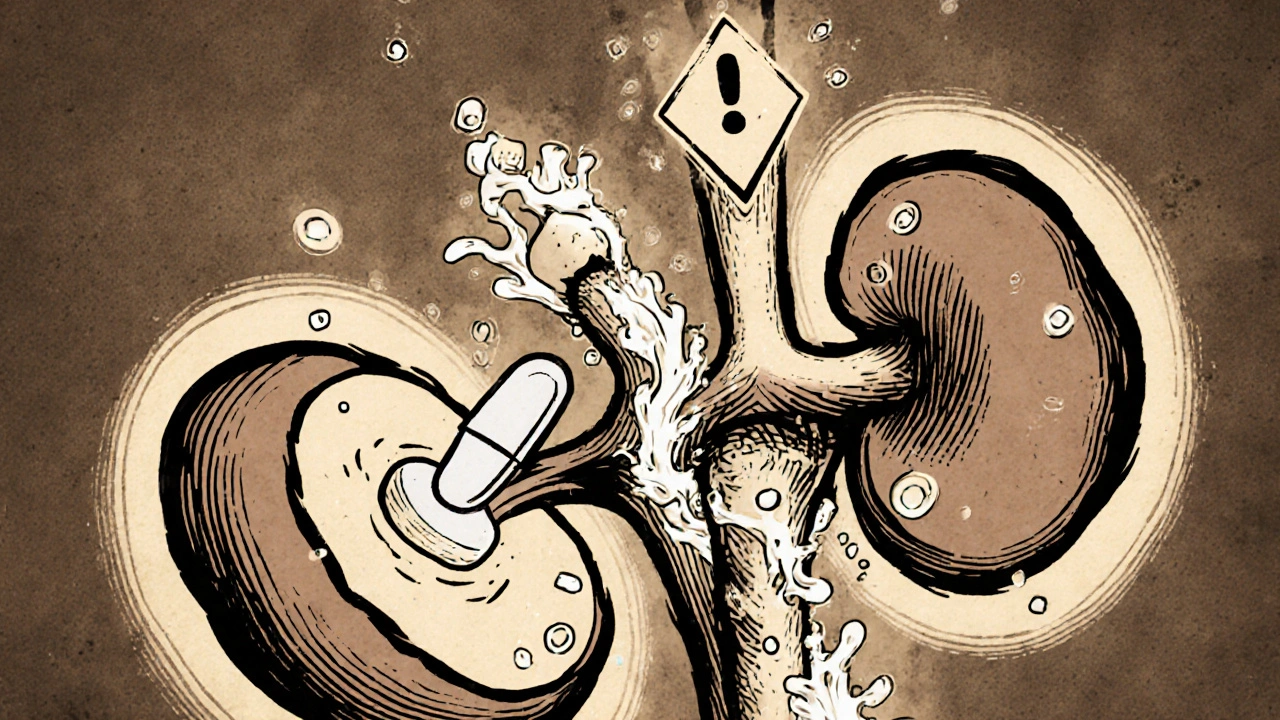
Metformin doesn’t make your pancreas produce more insulin. Instead, it helps your body use insulin better and reduces the amount of sugar your liver releases. It’s cheap, effective, and has been used for over 60 years. But here’s the catch: your kidneys clear metformin completely. No liver processing. No breakdown. Just filtered out by your kidneys and flushed in your urine.
When your kidneys are working normally, metformin leaves your body in about 6 to 8 hours. But if your kidney function drops-say, from an eGFR of 90 down to 40-the drug starts to stick around. That’s not dangerous by itself. But if something else stresses your body-like infection, dehydration, or heart failure-your cells might switch from using oxygen to burn sugar. That’s when they start making lactic acid.
Metformin makes this shift a little more likely. It interferes with how mitochondria (your cells’ power plants) use oxygen. So if your kidneys are slow and your body is under stress, metformin can push lactic acid levels up. That’s the real risk-not the dye, but the combination of poor kidney function + stress + metformin.
Contrast Dye and Kidney Damage: The Real Story
Contrast dye can cause a temporary dip in kidney function called contrast-induced acute kidney injury (CI-AKI). It’s more common in people with existing kidney problems, diabetes, or dehydration. But here’s the key point: CI-AKI is usually mild and reversible. In most cases, kidney function returns to normal within 2 to 3 days.
Studies tracking over 100,000 patients show that the risk of CI-AKI from IV contrast is less than 5% in people with mild kidney issues, and even lower in those with normal function. And in the vast majority of those cases, the kidney drop is so small it doesn’t even need treatment.
So why did we used to panic? Because early studies linked contrast dye to kidney damage and assumed that meant metformin would pile up and cause lactic acidosis. But later research-like a 2013 analysis in the PMC journal-showed that metformin-induced lactic acidosis almost never happens from contrast dye alone. The real danger comes from patients who already have multiple risk factors.
Current Guidelines: It’s Not One-Size-Fits-All
In 2016, the FDA changed its guidelines. So did the American College of Radiology and the National Kidney Foundation. The old rule-stop metformin for every scan-is outdated. Now, it’s based on your kidney function and your overall health.
Here’s what you need to know:
- eGFR above 60? You can keep taking metformin. No need to stop. Not even for heart catheterizations. The risk is negligible.
- eGFR between 30 and 60? Stop metformin at the time of the scan. Restart only after 48 hours, and only if your kidney function hasn’t dropped.
- eGFR below 30? Metformin is already not recommended. Don’t restart unless your doctor says so.
- Any procedure using arterial contrast? (Like cardiac cath or angioplasty) Stop metformin, no matter your eGFR. The dye goes directly into arteries, which can cause more kidney stress.
- Other risk factors? If you have heart failure, liver disease, severe infection, or drink alcohol heavily-talk to your doctor. You may need to pause metformin even if your eGFR is fine.
Why the difference between IV and arterial contrast? IV contrast spreads through your bloodstream slowly. Arterial contrast is injected directly into an artery-like the one feeding your heart. It hits the kidneys harder and faster. That’s why the risk is higher for procedures like angiograms.
What Happens If You Don’t Stop Metformin?
For most people, nothing. A 2021 study of over 20,000 patients found no cases of lactic acidosis in those who kept taking metformin during IV contrast scans-even if their eGFR was between 45 and 60.
But here’s the flip side: stopping metformin can be risky too. If you’re diabetic, going off your medication for 48 hours can spike your blood sugar. That’s dangerous. High blood sugar can lead to dehydration, which stresses your kidneys even more. It can also trigger diabetic ketoacidosis, especially in type 1 or advanced type 2 diabetes.
One hospital system in the UK found that before switching to the new guidelines, they were stopping metformin in 92% of patients getting contrast scans. After switching, they reduced that to 28%. No cases of lactic acidosis occurred. But they saw fewer hospital admissions for high blood sugar.
When to Restart Metformin After a Scan
Don’t just guess. Don’t restart after 48 hours just because “that’s what you heard.” You need a blood test.
After your scan, your doctor should check your kidney function with an eGFR test 48 hours later. If your eGFR is the same or better than before the scan, you can restart metformin. If it dropped significantly, your doctor will figure out why-dehydration? infection?-and treat that first.
And here’s something most people don’t know: you don’t need to check metformin levels in your blood. Lactic acidosis isn’t diagnosed by how much metformin is in your system. It’s diagnosed by your blood pH, lactate levels, and symptoms. By the time lactate is high enough to be dangerous, you’re already sick. Waiting for a metformin level test wastes time.

What If You Have Lactic Acidosis?
It’s rare, but if it happens, it’s serious. Symptoms include:
- Deep, rapid breathing (your body trying to blow off acid)
- Nausea, vomiting, stomach pain
- Feeling extremely weak or confused
- Low blood pressure, cold skin
If you have these symptoms after a scan, go to the ER immediately. Treatment is simple but urgent: stop metformin, give IV fluids, and start dialysis if needed. Hemodialysis removes both metformin and lactic acid from your blood. Studies show that patients who get dialysis within hours have survival rates over 80%. Those who wait? The death rate jumps to 40%.
Most cases happen in people over 65 with heart failure, infection, or chronic kidney disease. It’s not about the dye. It’s about being sick and having kidneys that can’t keep up.
What’s Changing Now? The Future of Metformin Safety
Doctors are moving toward personalized care. Research is starting to look at genetic factors-some people might have a natural tendency to build up lactic acid when on metformin. Others might clear it faster. In the next 5 years, we may see genetic tests used to tailor metformin use around procedures.
For now, the message is clear: don’t overreact. If your kidneys are okay and you’re not sick, keep taking metformin. If your kidneys are weak or you’re ill, pause it-but only after talking to your doctor. Don’t let fear of a 1-in-100,000 risk cause you to skip a needed scan or risk uncontrolled diabetes.
The old fear of metformin and contrast dye was based on theory, not data. Today’s guidelines are based on real-world outcomes. And the data says: you’re safer keeping your diabetes under control than you are stopping your medication.
Quick Checklist: What to Do Before Your Scan
- Check your latest eGFR result (from a blood test in the last 3 months).
- Are you on metformin? If yes, note the dose and how long you’ve been taking it.
- Do you have heart failure, liver disease, or a recent infection?
- Is the scan using IV contrast or arterial contrast?
- Ask your doctor: “Based on my kidney function and health, should I stop metformin?”
- After the scan, schedule a follow-up blood test for eGFR in 48 hours.
- Don’t restart metformin until your doctor confirms your kidneys are stable.
Metformin isn’t the enemy. Fear of it is. The real danger isn’t the contrast dye-it’s ignoring your kidney health, ignoring your diabetes, or letting outdated rules make you sick.


Stop metformin? Nah, my doc just told me to keep taking it. Kidneys are fine, scan went great.
I used to panic every time I had to get a CT scan. My endo finally sat me down and showed me the data-turns out, the real risk isn't the dye, it's dehydration and being sick. I started drinking water like it's my job before scans and honestly? My anxiety dropped 90%. People still treat metformin like it's radioactive, but it's just a drug that needs context. Your kidneys aren't a light switch-they're a filter. If they're working, let 'em work.
Ah yes, the classic pharmacokinetic myopia. We've conflated correlation with causation since the 80s-metformin + contrast = lactic acidosis, ergo, contraindication. But modern meta-analyses (e.g., PMC 2013, JAMA 2021) show negligible risk in eGFR >30 with no acute stressors. The real pathology here isn't pharmacological-it's institutional inertia. We're clinging to precautionary dogma like a security blanket while ignoring evidence-based nuance. 🤷♂️
Why are we even still talking about this? In America we got better things to worry about than stopping metformin. My cousin got a CT with dye and didn't stop her meds-she’s fine. Stop overthinking it. #AmericanCommonSense
I’ve been on metformin for 12 years. Got a coronary angiogram last year-eGFR was 58. Doc said stop. I asked why. He said 'because that’s what the old protocol says.' I showed him the 2021 study. He paused. Then said, 'You’re right. Just keep taking it.' That’s the problem-guidelines lag behind science by decades. Doctors aren’t lazy, they’re overwhelmed. But we need to push for better education. Also, don’t forget: lactic acidosis isn’t about metformin concentration. It’s about pH and lactate. Check those. Not your metformin level. That’s a waste of time.
Let’s be brutally honest: the medical establishment’s reluctance to update guidelines isn’t about safety-it’s about liability. If you stop metformin and the patient has a bad sugar spike, you get sued. If you don’t stop it and they get lactic acidosis (even if it’s from sepsis), you get sued harder. So the safe play is always to follow the outdated rule. The data doesn’t matter when the legal system rewards fear. That’s not medicine. That’s risk management dressed in a white coat.
In India, we’ve been quietly doing this for years-no blanket stoppage unless eGFR <30 or acute illness. Our hospitals are overloaded, and we can’t afford to disrupt diabetes control for every scan. The data is clear: lactic acidosis from contrast is a myth in stable patients. We’ve seen patients with eGFR 45 get angiograms, keep metformin, and walk out fine. The real enemy? Lack of access to follow-up creatinine tests. If you can’t check kidney function 48 hours later, then yes, err on caution. But if you can? Trust the numbers, not the fear.
I’m not a doctor but my mom’s on metformin and she got a kidney ultrasound with dye last month. She didn’t stop it. No issues. Honestly, I think we’ve turned a simple med into this scary monster because we don’t understand how kidneys work. Just drink water. Check your labs. Talk to your doc. Done.
This is why we need patient education. So many people are terrified to get necessary scans because they think metformin is poison. The truth? Uncontrolled diabetes is far more dangerous than a 0.01% risk of lactic acidosis. I’ve seen patients delay cardiac imaging for months because they were scared to restart metformin. Don’t let fear make you sicker than the condition you’re trying to treat. You’re not a lab rat-you’re a human being with a life to live. Keep your glucose in check. That’s the real win.
Okay but like… why do we still even have this rule? 😅 I got my CT last week, didn’t stop metformin, and my doc didn’t even blink. Like, we’re in 2025. Can we please stop treating meds like they’re haunted? 🙃
There’s a deeper philosophical layer here. We treat medical guidelines as immutable laws, but medicine is a living science. The shift from 'always stop' to 'context-dependent' reflects a broader evolution in how we conceptualize risk: from binary thinking (safe/dangerous) to probabilistic reasoning (risk gradients). Metformin isn’t inherently dangerous-it’s a tool. And tools are judged not by their nature, but by their use. The real failure isn’t in the drug-it’s in our refusal to adapt our cognitive frameworks to new data. We fear what we don’t understand. And we fear change more than we fear disease.
I work in radiology. We used to stop metformin for every single patient-no questions asked. Then we started tracking outcomes. Over 18 months, we had zero cases of lactic acidosis in patients who kept metformin with eGFR >30. Meanwhile, we had three hospitalizations for hyperglycemia because people stopped their meds. We changed our protocol. No drama. No lawsuits. Just better care. The biggest obstacle isn’t science-it’s the stubbornness of people who think 'we’ve always done it this way' is a valid reason. It’s not. It’s laziness with a badge.
bro why are we even doing this? just stop the metformin. why risk it? i dont wanna be that guy who dies because he was too cool for the rules 😭
The FDA’s 2016 revision was a dangerous precedent. It prioritized convenience over caution. While the statistical risk may be low, the consequence is catastrophic. One death is one too many. We must not normalize deviating from established protocols without overwhelming, reproducible, multi-center evidence. The burden of proof lies with those advocating change-not those preserving safety.
EVERYONE KNOWS THE PHARMA COMPANIES PUSHED THIS CHANGE TO MAKE MORE MONEY!! THEY DON’T WANT YOU STOPPING METFORMIN BECAUSE THEN YOU’D HAVE TO BUY MORE OF IT!! AND THE DOCTORS? THEY’RE IN ON IT!! THEY’RE PAID BY BIG PHARMA TO IGNORE THE TRUTH!! YOU THINK THEY REALLY WANT YOU TO CHECK YOUR KIDNEYS AFTER THE SCAN? NO!! THEY JUST WANT YOU TO RESTART AND KEEP BUYING!!
i heard someone say metformin makes your kidneys weak? is that true? i think i should stop it even if my eGFR is fine just in case. better safe than sorry right?
Honestly? I think the real villain here is the medical-industrial complex’s obsession with checklists over critical thinking. We’ve turned patient care into a fill-in-the-blank form. 'eGFR >60? Check. Scan type? Check. Stop metformin? No.' But what about the patient’s hydration status? Their recent fever? Their history of heart failure? No field for that. So we default to the checkbox. And that’s not medicine-it’s administrative theater. The patient’s body doesn’t care about your algorithm. It cares about your attention.