If you’re taking a calcium channel blocker for high blood pressure, and you love your morning glass of grapefruit juice, you might be at risk-without even realizing it. This isn’t just a vague warning you hear from your pharmacist. It’s a well-documented, potentially life-threatening interaction that affects grapefruit and certain blood pressure medications. And it doesn’t matter if you take your pill hours after drinking the juice. The damage is already done.
Why Grapefruit Is a Problem for Blood Pressure Meds
Grapefruit isn’t just a tart, refreshing fruit. It’s packed with chemicals called furanocoumarins-specifically 6',7'-dihydroxybergamottin and bergamottin. These compounds shut down an enzyme in your gut called CYP3A4. That enzyme is responsible for breaking down certain drugs before they enter your bloodstream. When it’s blocked, the drug doesn’t get processed the way it should. Instead, it floods into your system at levels you didn’t intend. For calcium channel blockers like felodipine, that means your blood levels can jump 3 to 5 times higher than normal. One study showed that a standard 10 mg dose of felodipine, when taken with grapefruit juice, produced blood concentrations equivalent to taking 30-50 mg. That’s not a small tweak. That’s a dangerous overdose. And here’s the kicker: one 200 ml glass of grapefruit juice-about one small glass-is enough to cause this effect. It doesn’t take a whole pitcher. And once the enzyme is turned off, it stays off for up to 72 hours. That means if you drink grapefruit juice on Monday morning, and take your pill on Tuesday night, you’re still at risk.Which Calcium Channel Blockers Are Most Affected?
Not all calcium channel blockers react the same way. The ones most at risk are the dihydropyridines-especially:- Felodipine (Plendil): The most sensitive. Bioavailability can increase by up to 500%.
- Nicardipine (Cardene): Strong interaction, similar to felodipine.
- Nimodipine (Nymalize): Used for brain vessel spasms; grapefruit can push levels into toxic range.
- Pranidipine: Less common, but still risky.
- Amlodipine (Norvasc): Still interacts, but less dramatically. Still not safe.
What Happens When the Interaction Occurs?
When too much calcium channel blocker hits your bloodstream, your blood pressure can crash. You might feel dizzy, lightheaded, or faint. Your heart may race as your body tries to compensate. Swelling in your ankles and feet-common side effects of these drugs-can become severe. In older adults, this can lead to falls, fractures, or even hospitalization. Dr. Amelie Hollier, a nurse practitioner, shared a real case from her practice: an elderly woman took her amlodipine with grapefruit juice every morning. Within days, she couldn’t stand without help. Her dose was 10 mg. The grapefruit turned it into the equivalent of 25 mg. She ended up in the ER with dangerously low blood pressure. These aren’t rare cases. The CDC estimates that grapefruit-related drug interactions send about 15,000 people to U.S. emergency rooms every year. Most of them are on blood pressure meds.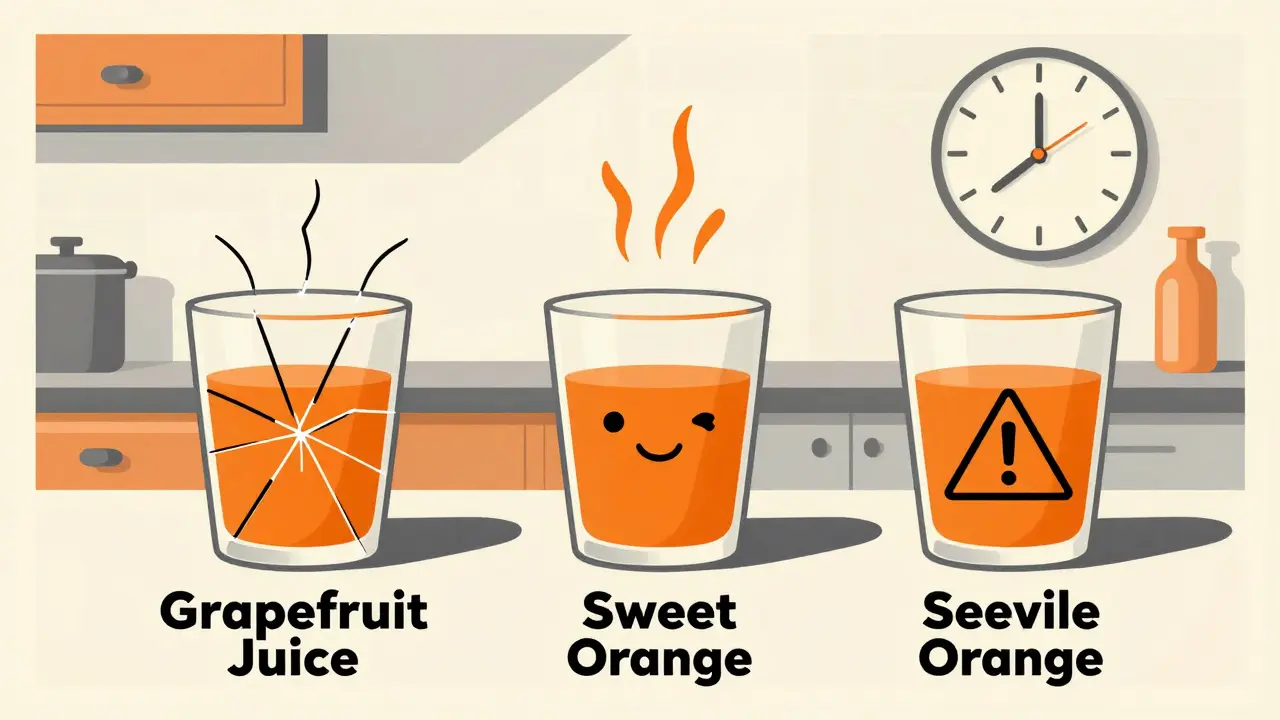
Other Citrus Fruits: Are They Safe?
Not all citrus is created equal. Grapefruit is the worst offender because of its high concentration of furanocoumarins-up to 10 mg per 100 ml. Sweet oranges, like navel or Valencia, have almost none. So, a glass of regular orange juice? Generally safe. But here’s where people get confused:- Seville oranges (used in marmalade): High in furanocoumarins. Avoid.
- Tangelos (a grapefruit-orange hybrid): Also risky. Contains enough of the bad compounds to cause problems.
- Orange juice from concentrate: Usually safe if it’s made from sweet oranges. But check the label-if it says “grapefruit blend” or “citrus blend,” skip it.
What Should You Do Instead?
If you’re on a calcium channel blocker, the safest move is to eliminate grapefruit and its close relatives from your diet entirely. That includes:- Grapefruit juice (even “low-sugar” or “no pulp” versions)
- Whole grapefruit
- Grapefruit segments in salads
- Smoothies containing grapefruit
- Seville orange marmalade
- Tangelos or pomelos
What If You’re Already Taking One of These Drugs?
If you’ve been drinking grapefruit juice and taking your blood pressure pill together, stop immediately. Don’t wait for symptoms. Talk to your doctor or pharmacist. They can:- Check which specific drug you’re on and its risk level
- Switch you to a safer alternative
- Monitor your blood pressure more closely for a few days
- ACE inhibitors like lisinopril
- ARBs like valsartan
- Thiazide diuretics like hydrochlorothiazide
- Some beta blockers like metoprolol




So let me get this straight - you’re telling me I can’t have my morning grapefruit juice with my felodipine, but I can drink orange juice while skydiving off a cliff? That’s not a drug interaction, that’s a culinary assassination plot.
And yet, the FDA still lets juice companies slap ‘100% natural’ on bottles that could turn your amlodipine into a fireworks display. Brilliant.
Also, why is this not a black box warning? If grapefruit were a person, it’d be in prison by now.
I used to drink grapefruit juice every day like it was water - I thought it was ‘healthy’ because it was citrus. Turns out, my body was basically doing a slow-motion version of that scene in The Matrix where Neo sees the code.
After my doctor told me to stop, I switched to tangerines and now I feel like a new person. No more dizziness. No more ‘why is the floor tilting?’ moments. I even started a little citrus journal - sweet oranges on Mondays, lemons on Wednesdays, mandarins on Fridays. It’s my tiny ritual of self-care now.
It’s not about deprivation. It’s about choosing a version of yourself that gets to wake up and stand up without feeling like you’re about to faint into your cereal.
And honestly? The tangerines taste better anyway. Less bitter. More joy. That’s what healing looks like - not in pills, but in peel.
As a nurse practitioner, I see this every single week. Patients come in with BP readings so low their monitors beep like a dying alarm clock. They say, ‘But I only had one glass!’ - and I say, ‘Yeah, and one glass is all it takes to silence your liver’s detox switch for three days.’
It’s not about fear-mongering. It’s about precision. Your meds are calibrated for your metabolism. Grapefruit? It’s like throwing a wrench into a Swiss watch.
And don’t get me started on ‘I take it at night, juice in the morning’ - that’s not a strategy, that’s Russian roulette with a citrus bullet.
Teach your parents. Teach your grandparents. This isn’t a ‘maybe’ - it’s a ‘please don’t die’.
grapefruit is a traitor. it looks innocent. it smells fresh. it tastes like rebellion. but inside? it’s a silent assassin with a PhD in pharmacology.
my grandma died from this. she didn’t even know. she just liked her juice. now i put a sticky note on my fridge. it says: ‘this is not your friend.’
Man, I used to love grapefruit juice with my breakfast - it felt so ‘adult’ and ‘healthy.’ Then I started on amlodipine and my ankles swelled up like I was auditioning for a balloon animal convention.
Switched to orange juice and boom - no more puffiness. No more dizzy spells. Just me, my toast, and my peace of mind.
Also, lemme just say - if you’re still drinking grapefruit juice with your meds, you’re not being ‘edgy,’ you’re just being a walking clinical trial. And nobody wants to be the test subject.
Ah, the tragicomedy of modern pharmacology - where a fruit, once a symbol of exotic indulgence, has become the silent executioner of the middle-aged bourgeoisie.
We have reduced the sublime art of breakfast to a bureaucratic footnote in a pill bottle. The grapefruit, once the crown jewel of Mediterranean mornings, now bears the weight of our collective medical ignorance.
Is it not poetic? That the very essence of vitality - citrus, sunlight, dawn - should be the agent of our pharmacological undoing?
And yet… we persist. We sip. We rationalize. We say, ‘It’s just once.’
But the CYP3A4 enzyme does not forgive. It does not forget. It is not moved by your intentions.
So tell me - is your juice a ritual of life… or a quiet elegy for your coronary arteries?
STOP BEING SOFT. If you can’t give up grapefruit juice, you don’t deserve to live with high blood pressure. You think your ‘one glass’ is harmless? You’re not special. You’re a walking ER visit waiting to happen.
My uncle died from this. He was 72. He swore he ‘only had it on weekends.’ Guess what? His heart didn’t care about his schedule.
Stop being a victim. Stop being a victim of your own taste buds. If your meds say no grapefruit - then no grapefruit. End of story. No drama. No ‘but I love it.’
Grow up.
You’re all overthinking this. Grapefruit = bad. Orange = good. That’s it. If you need a 1000-word essay to understand that, you shouldn’t be managing your own meds.
Just don’t drink it. Done.
Look, I get it - you love your citrus. I do too. But here’s the thing: your body doesn’t care if you’re ‘trying to be healthy.’ It cares about enzymes, bioavailability, and whether your blood pressure just dropped to ‘I-can’t-stand-up’ levels.
I had a friend who swore he was fine because he drank grapefruit juice at night. He woke up in the ER with a heart rate of 140. He didn’t even know what a CYP3A4 enzyme was.
So here’s my advice: stop being a hero. Stop being a rebel. Just… switch to orange juice. It’s cheaper. It’s sweeter. And your heart will thank you in a language you can’t argue with.
And if you’re still not convinced? Go read the CDC stats. 15,000 people a year. That’s not a statistic. That’s your neighbor. Your aunt. Your dad.
Be smart. Not stubborn.
I’ve been on diltiazem for years and never knew grapefruit was even a thing. My pharmacist mentioned it once - I thought they were joking. Turns out, I was the joke.
Switched to mandarins. Now I eat them like candy. My BP is stable, I sleep better, and I don’t feel like I’m going to pass out when I stand up.
Also, I made a little chart for my fridge: ‘Safe Citrus’ vs ‘Danger Zone.’ It’s colorful. It’s fun. And it saved my life. Who knew health advice could be this… aesthetic?
While the clinical data regarding furanocoumarin-mediated CYP3A4 inhibition is robust and well-replicated, the public health messaging remains fundamentally flawed. The emphasis on grapefruit as a singular villain obscures the broader issue: pharmacovigilance in ambulatory care is catastrophically under-resourced.
It is not sufficient to rely on patient recall or pharmacist warnings when the average primary care encounter lasts 7.3 minutes. The onus should not be on the patient to memorize pharmacokinetic interactions - it should be on the prescriber to select non-interacting alternatives when feasible.
Moreover, the continued availability of grapefruit juice in hospital cafeterias and outpatient clinics constitutes a systemic failure of institutional safety protocols.
This is not a dietary advisory - it is a structural flaw in the delivery of pharmacotherapy.
Adam, I just read your comment - and you’re absolutely right. We’re putting the burden on patients when we should be redesigning the system.
My clinic just started putting ‘GRAPEFRUIT WARNING’ stickers on every prescription bottle for calcium channel blockers. We also added a checkbox in the EHR: ‘Patient counseled on citrus interaction.’
It’s small. But it’s something.
Thank you for saying what needs to be said. This isn’t just about juice. It’s about how we care - or fail to care - for people who just want to live without fear.