When your stomach suddenly locks up in sharp, unrelenting pain-right under your ribs, lasting hours, then vanishing just as fast-you might think it’s indigestion. But if this keeps happening, especially after fatty meals, it could be gallstones. Most people don’t know they have them until the pain hits. And when it does, it’s not something you can just sleep off.
What Happens When Gallstones Block the Flow
Gallstones are hard deposits that form in the gallbladder, usually made of cholesterol or bilirubin. About 10-15% of adults in developed countries have them, but 80% never feel a thing. The problem starts when one of these stones gets stuck-usually in the cystic duct, the tube that lets bile leave the gallbladder. That’s when biliary colic kicks in. The pain isn’t crampy or relieved by burping or pooping. It’s steady, intense, and centered in the upper right side of your belly or just below your breastbone. It hits fast, peaks within an hour, and can last anywhere from one to five hours. Once the stone moves or shifts, the pain fades. But it doesn’t mean the problem is gone. In fact, the American Academy of Family Physicians found that more than 90% of people who have one episode of biliary colic will have another within ten years. Two out of three will have a repeat attack within just two years.When Biliary Colic Turns Dangerous
Biliary colic is painful, but it’s not always dangerous. The real risk comes when the blockage doesn’t clear. If the stone stays stuck for more than a few hours, the gallbladder starts to swell and get inflamed. That’s acute cholecystitis. It’s not just pain anymore-it’s fever, nausea, vomiting, and tenderness so bad you can’t even breathe deeply. About 20% of biliary colic episodes turn into this. If the stone slips into the common bile duct, things get even worse. You might turn yellow (jaundice), your urine turns dark, and your stools turn pale. This means bile can’t reach your intestines. It can also trigger pancreatitis, a dangerous inflammation of the pancreas. The NHS reports that without treatment, 20-30% of people with symptomatic gallstones end up in the emergency room within five years.What Causes Gallstones in the First Place
It’s not just eating too much fat. Gallstones form when your bile gets out of balance. Cholesterol stones make up 80% of cases in places like the U.S. and New Zealand. Your liver dumps too much cholesterol into bile, and it hardens into crystals. Pigment stones, made of bilirubin, are less common and often linked to liver disease or blood disorders. Some people are more at risk. Women are two to three times more likely to get them than men. Being overweight or obese raises your risk-especially with rapid weight loss. Age matters too. After 40, your chances climb. And if you’re Hispanic, your risk is 45% higher than non-Hispanic whites, according to the 2023 National Health and Nutrition Examination Survey.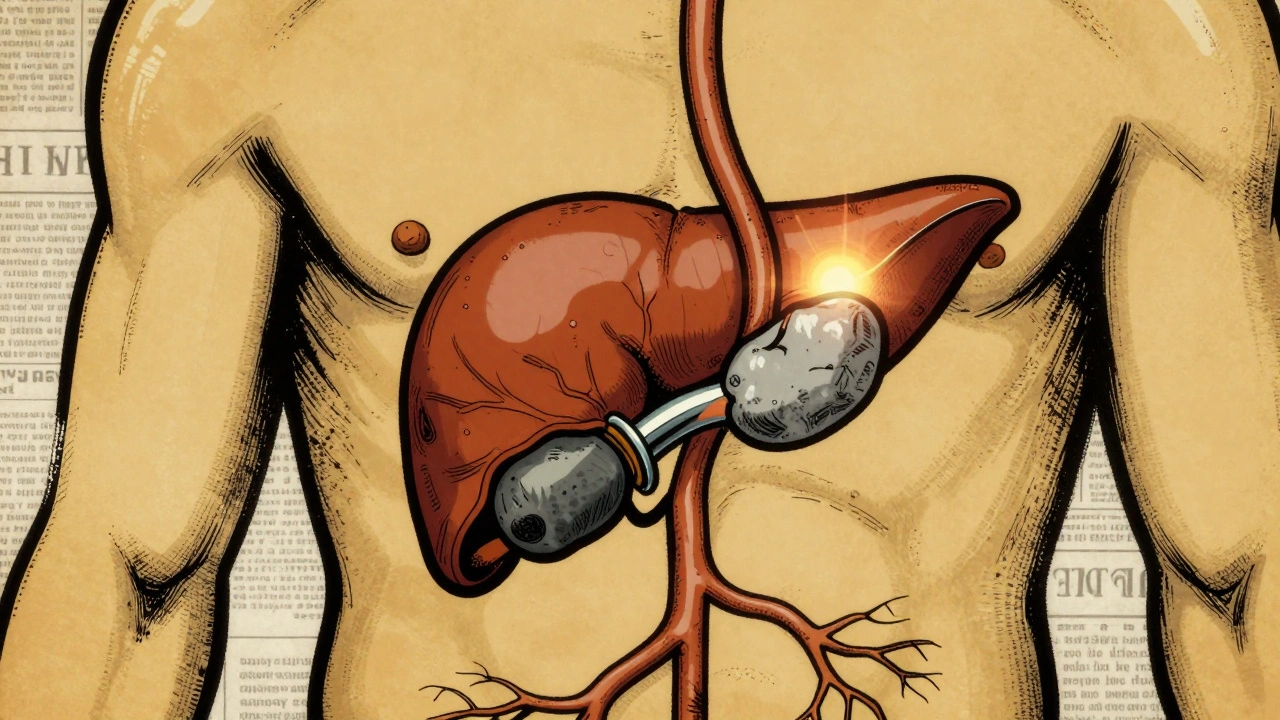
Surgery: The Only Real Fix
There’s no magic pill that reliably gets rid of gallstones. Medications like ursodeoxycholic acid can dissolve small cholesterol stones-but only in about 30-50% of cases, and it takes months. Even then, half the people who get relief see the stones come back within five years. Shock-wave therapy to break up stones? It’s rarely used now because stones return too often. That’s why surgery is the standard. Removing the gallbladder-cholecystectomy-isn’t just common; it’s the most effective solution. About 700,000 of these surgeries are done in the U.S. every year. In New Zealand and other developed countries, over 90% are done laparoscopically. That means four small cuts, a tiny camera, and tools that remove the gallbladder in about 45-60 minutes. Recovery is quick. Most people go home the same day or the next. You’re up and walking within hours. Pain is mild compared to the old open surgery, which needed a big cut and weeks of recovery. Now, most people are back to normal in about a week. Studies show 82% of patients say their quality of life improved dramatically after surgery.When Surgery Isn’t the Best Choice
Surgery isn’t risk-free. For healthy people under 75, the chance of serious complications is less than 2%. But for older adults with heart disease, diabetes, or other health problems, the risk jumps. A 2023 study in the Annals of Surgery found that for patients over 75 with three or more chronic conditions, the 30-day death rate after surgery rose to 2.8%-up from just 0.1% in healthy patients. That’s why doctors don’t rush into surgery for everyone. If you’re 80, have severe lung disease, and only get pain once every few months, watchful waiting might be smarter. But if you’re 50, active, and your pain keeps coming back? Surgery is the clear choice. The Society of American Gastrointestinal and Endoscopic Surgeons says if you’re diagnosed with acute cholecystitis, you should have surgery within 72 hours. Waiting longer increases the chance the surgeon will have to switch from laparoscopic to open surgery-from 7% to 25%.



I had my gallbladder out last year after 3 years of 'indigestion' that kept getting worse. One minute I'm fine, next I'm curled up on the floor like someone kicked me in the ribs. Surgery was a breeze. Went home the same day. Now I eat pizza like it's my job. 🍕
OMG YES SAME 😭 I thought it was stress or bad tacos... until I cried in the ER at 2am. Ultrasound showed 12 stones. Got removed 2 weeks later. Best decision ever. No more fear of dinner. 🙌
soooo... you're telling me the entire medical industry just decided to cut out perfectly good organs because people can't stop eating cheeseburgers? 🤔
It's important to note that while surgery is the gold standard, not everyone needs it immediately. For asymptomatic cases, especially in older adults or those with high surgical risk, monitoring is valid. But if you're having recurrent pain - yes, don't wait. The data is clear.
People who wait until they're vomiting and jaundiced are basically asking for a 6-hour surgery and a month of recovery. You knew something was wrong for months. You ignored it. Now you're mad the system is 'too aggressive'? No. You're just mad you didn't listen to your body.
Did you know the gallbladder is linked to the liver's detox pathways? And that glyphosate in processed foods causes bile to thicken? They don't tell you this because Big Pharma makes billions off cholecystectomies. 🤫
There's a deeper question here: why do we treat the symptom instead of the cause? If bile imbalance is the root, why aren't we researching dietary interventions that restore bile flow naturally? We jump to removal because it's profitable, not because it's holistic.
I remember my first attack like it was yesterday. I thought I was dying. Then I got the ultrasound and the doctor said, 'Oh, you've got stones.' I said, 'So... what do I do?' He shrugged. 'Well, you could try not eating fat.' I said, 'I'm not giving up tacos.' So I had surgery. Best. Choice. Ever. Now I eat tacos every day. No pain. Just joy.
I had the pain for 5 years. Went to 7 doctors. 4 said it was anxiety. 2 said it was IBS. The 7th said 'you need your gallbladder out' and I cried. I was 28. My mom said 'you're too young for that.' I said 'I'm too young to keep screaming in the bathroom.' Surgery saved my life. And my social life.
If you're overweight and get these attacks try eating smaller meals more often and avoid fried stuff. Also drink lemon water in the morning. It helps bile flow. I did this for 6 months and my attacks stopped. But if they come back, don't be stubborn. Get it checked
i mean yeah surgery is great but like... what if you dont have insurance? or you live in a town with no good surgeons? or you're scared of anesthesia? its not just 'get it done' for everyone. some of us are stuck waiting because life is hard. dont judge.
I've read the same article three times. The statistics are misleading. The '82% improved quality of life' - that's from a study funded by the American College of Surgeons. And the '20-30% end up in ER' - that's over five years, but they didn't account for people who changed their diet. The real danger? Misinformation disguised as medical advice.
This is so helpful. In Nigeria, many people don't even know what gallstones are. They think it's spiritual. I showed this to my cousin - she had pain for 2 years. Went to clinic yesterday. Ultrasound confirmed stones. Now she's scheduled for surgery. Thank you for writing this clearly.