When you pick up a prescription and see a generic drug on the label, you might assume it’s just a cheaper version of the brand-name pill. But behind that simple switch is a highly regulated, science-driven process that’s been keeping millions of Americans healthy and saving the U.S. healthcare system billions each year. The FDA doesn’t just approve generics because they’re affordable-it approves them because they must work exactly the same way as the original drug. And the legal foundation for that approval? It’s the Hatch-Waxman Act of 1984.
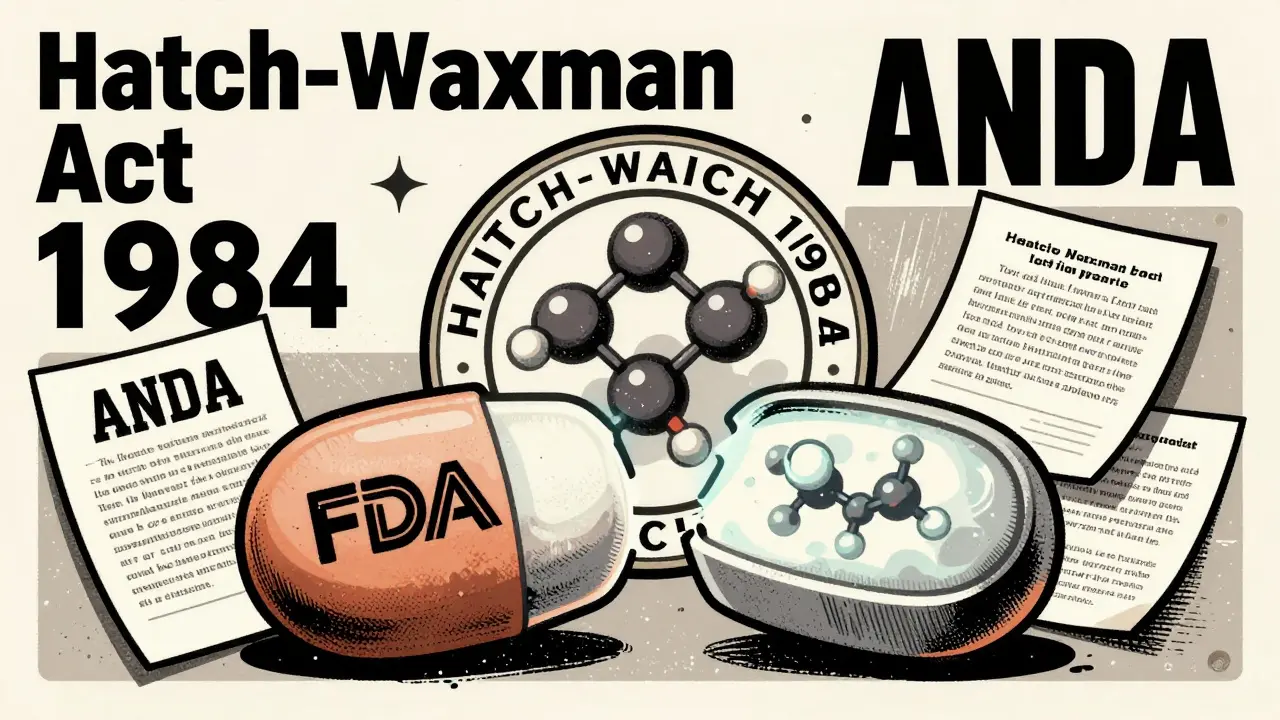
The Hatch-Waxman Act: The Legal Backbone of Generic Drugs
Before 1984, bringing a generic drug to market meant repeating every single clinical trial the brand-name company had done. That was expensive, slow, and discouraged competition. The Drug Price Competition and Patent Term Restoration Act, better known as the Hatch-Waxman Act, changed everything. Passed on September 24, 1984, this law created the Abbreviated New Drug Application (ANDA) pathway under Section 505(j) of the Federal Food, Drug, and Cosmetic Act. The word “abbreviated” is key here. Generic manufacturers don’t need to prove safety or effectiveness from scratch. Instead, they rely on the FDA’s prior findings for the brand-name drug, called the Reference Listed Drug (RLD). This single change turned generic drug development from a near-impossible task into a viable business. Today, nearly 9 out of 10 prescriptions filled in the U.S. are for generic drugs. That’s not luck-it’s the result of a carefully designed legal framework that balances innovation with access.What the FDA Actually Requires for Approval
The FDA doesn’t lower its standards for generics. In fact, the requirements are just as strict-just different. To get approved, a generic drug must meet five core criteria:- Same active ingredient(s) as the brand drug
- Same strength, dosage form, and route of administration
- Same intended use or indications
- Same bioequivalence profile
- Same manufacturing quality standards
The ANDA Submission: What’s Inside the Application
An ANDA isn’t a simple form. It’s a detailed dossier that includes:- Chemistry, Manufacturing, and Controls (CMC) data-showing how the drug is made, tested, and packaged
- Facility information-every site where the drug is produced, tested, or packaged must be inspected by the FDA
- Proposed labeling-identical to the brand drug’s, with no misleading claims
- Bioequivalence study reports-raw data, protocols, and statistical analysis
Timeline and Review Process: From Submission to Approval
The FDA doesn’t take years to review generics anymore. Thanks to the Generic Drug User Fee Amendments (GDUFA), first launched in 2012 and renewed through GDUFA III in 2022, there are clear performance goals.- Standard ANDAs: reviewed within 10 months of submission
- Priority ANDAs (like first generics or drugs in shortage): reviewed within 8 months
Why Generics Cost 80-85% Less
It’s not because they’re made cheaper. It’s because they don’t have to pay for the original research. Developing a new brand-name drug costs an estimated $2.6 billion on average. That includes failed drugs, clinical trials, marketing, and patent protection. Generics don’t carry that burden. Their development costs are typically between $1 million and $5 million. That’s why they can sell for 80-85% less. But here’s the catch: the savings don’t come from cutting corners. The FDA requires the same quality controls, same inspections, same testing. The cost difference is purely in R&D. When multiple generics enter the market, competition drives prices even lower. In some cases, a 30-day supply of a generic drug costs less than a co-pay for the brand.Challenges with Complex Generics
Not all drugs are easy to copy. Simple pills? Easy. Inhalers? Not so much. Topical creams? Harder. Extended-release tablets? Very hard. These are called complex generics. They don’t just need bioequivalence-they need proof that the drug behaves the same way in the body under real-world conditions. For example, a generic inhaler must deliver the same particle size and lung deposition as the brand. A generic topical cream must penetrate the skin at the same rate. The FDA has a dedicated initiative called Complex Generic Drug Product Development Resources to help manufacturers navigate these challenges. In 2023, the agency approved the first generic of Vivitrol, an extended-release injectable for opioid addiction. That approval was a big deal-not just because it was complex, but because it expanded access during a public health crisis.Who Makes These Drugs? The Market Players
The generic drug market is dominated by a few big names: Teva, Sandoz, Viatris (which merged Mylan and Pfizer’s generics division), and Amneal. But there are hundreds of smaller companies too, especially those specializing in complex generics or hard-to-make drugs. The Orange Book, officially called the “Approved Drug Products with Therapeutic Equivalence Evaluations,” lists every approved generic and brand drug, along with patent and exclusivity info. It’s the roadmap for when a generic can legally enter the market. In 2022, the U.S. generic drug market was worth about $125 billion. That’s not a small slice of the pie-it’s the whole table.
What’s Changing Now? The U.S. Manufacturing Push
On October 3, 2025, the FDA announced a new pilot program to speed up reviews for generic drugs made and tested in the United States. The goal? Strengthen the domestic supply chain. After years of relying on overseas manufacturing-especially for active ingredients-the U.S. government wants more production at home. Companies that test and manufacture their generics in the U.S. will get priority review. It’s a financial incentive wrapped in public health policy. The FDA hopes this will reduce reliance on foreign suppliers and prevent future drug shortages.Why This Matters to You
If you’re taking a generic drug, you’re not getting second-best. You’re getting the same medicine, approved under the same rules, made in the same kind of facilities, and held to the same standards. The FDA doesn’t treat generics as a second option. They’re the standard for affordability and access. For patients, that means lower co-pays. For the system, it means billions saved each year. For public health, it means more people can afford life-saving medications. The system isn’t perfect. Patent thickets still delay entry. Complex drugs still take longer. But the framework-the Hatch-Waxman Act, the ANDA pathway, the GDUFA reviews-is working. It’s delivering on its promise: high-quality, affordable drugs for everyone.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires that generic drugs meet the same strict standards for safety, strength, quality, and purity as brand-name drugs. Every generic must prove bioequivalence-meaning it works the same way in the body. The FDA inspects manufacturing sites for both brand and generic drugs using the same criteria.
Why do generic pills look different from brand-name pills?
U.S. law requires generic drugs to look different from brand-name versions to avoid trademark infringement. That means the shape, color, or markings may vary. But the active ingredient, dosage, and effectiveness are identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect how the drug works.
Can a generic drug fail to work for me?
If you’ve taken a brand-name drug without issues and then switch to a generic, it should work the same. The FDA requires bioequivalence, so the drug enters your bloodstream at the same rate and amount. Rarely, some people report differences-often due to inactive ingredients causing minor reactions. If you notice a change, talk to your doctor or pharmacist. It’s not the active ingredient failing-it might be a sensitivity to something else in the pill.
How long does it take for a generic to be approved?
Under current FDA guidelines, standard ANDA applications are reviewed within 10 months. Priority applications-like first generics or drugs in shortage-are reviewed in 8 months. The timeline starts after the FDA accepts the application for review. Many applications are rejected or delayed on the first try, especially if they’re incomplete or lack clear bioequivalence data.
What is a Paragraph IV certification?
A Paragraph IV certification is a legal statement a generic manufacturer files with its ANDA, claiming that a brand-name drug’s patent is invalid, unenforceable, or won’t be infringed. If the brand company sues for patent infringement, the FDA can’t approve the generic for up to 30 months. This is often used strategically to challenge patents and enter the market earlier, but it can delay generic availability.
Are all generics made in the U.S.?
No. Many generic drugs, especially active ingredients, are manufactured overseas-primarily in India and China. But the FDA inspects all facilities, whether domestic or foreign. The FDA’s new 2025 pilot program gives faster review to generics made and tested in the U.S., aiming to boost domestic production and reduce supply chain risks.
What’s the difference between a generic and a biosimilar?
Generics are copies of small-molecule drugs made with chemical synthesis. Biosimilars are copies of large, complex biologic drugs made from living cells. Biosimilars follow a different approval pathway under the BPCIA, not the ANDA process. They require more testing because biologics are harder to replicate exactly. A generic drug for metformin is not the same as a biosimilar for insulin.



Whoa. This is the kind of deep-dive that makes you actually respect the FDA instead of just yelling at them when your prescription costs too much. The Hatch-Waxman Act wasn’t just legislation-it was a quiet revolution. Imagine if every industry had to prove their copy worked as well as the original before selling it. We’d have way fewer junk apps and knockoff sneakers that fall apart after two walks.
And bioequivalence? 20% variance? That’s tighter than my ex’s grip on our shared Netflix account. The fact that they test this on actual humans with blood draws? That’s not bureaucracy-that’s science with a conscience.
Generics aren’t cheap because they’re bad. They’re cheap because the system finally stopped making the same guy pay for everyone’s R&D. It’s like letting the whole neighborhood use the same lawnmower instead of each buying a $2000 model. Genius.
Let’s be real-this whole ‘same bioequivalence’ narrative is corporate propaganda. The 20% window is a joke. Two drugs can be ‘bioequivalent’ and still have wildly different pharmacokinetics in real patients. I’ve seen patients on generic levothyroxine crash because the fillers altered absorption. The FDA doesn’t test for real-world variability, just lab conditions. This isn’t science-it’s regulatory theater.
And don’t get me started on ‘same manufacturing standards.’ Sure, the FDA inspects. But how many of those plants are in India with 200% overtime and zero whistleblower protections? The system is rigged to favor volume over safety. You think they’re checking every batch? Please.
While I appreciate the thoroughness of this exposition, one must acknowledge that the entire ANDA framework is predicated upon a fundamentally flawed epistemological assumption-that chemical identity equates to therapeutic equivalence. The pharmacodynamic variance in inactive ingredients, particularly in extended-release formulations, is not statistically insignificant, and yet the FDA continues to enforce a binary approval paradigm that ignores patient-specific pharmacogenomic responses. This is not healthcare-it is industrial standardization masquerading as medicine.
Furthermore, the GDUFA user fees create a perverse incentive structure wherein the agency prioritizes speed over scrutiny, effectively commodifying therapeutic outcomes. One cannot help but notice the irony: the same institution that demands double-blind trials for novel agents permits generic manufacturers to bypass clinical validation entirely under the guise of ‘abbreviated’ review. This is not progress-it is regulatory capture.
I switched to generic blood pressure meds last year and my co-pay dropped from $80 to $4. I didn’t feel any different. My doctor said it’s the same stuff. I trust her. Honestly I don’t care if it’s made in India or Ohio as long as it keeps me alive. Thanks for explaining how it works though. I always wondered why they looked so weird.
Generics are the silent revolution. The quiet rebellion against corporate greed. The unassuming hero in the pill bottle. We don’t celebrate them. We don’t give them parades. But every morning, millions swallow them without knowing they’re holding the key to a more just healthcare system.
The Hatch-Waxman Act didn’t just change laws-it changed lives. It said: your life is not a commodity. Your health is not a patent. And if you’re poor? You still deserve the same medicine. That’s not policy. That’s morality in tablet form.
They call it a generic. I call it dignity.
One thing people forget is that a lot of generics are made by the same companies that make brand names. Pfizer makes their own generics. So when you think you’re fighting Big Pharma by choosing generic, you might just be paying less to the same guys. The real villain isn’t the generic manufacturer-it’s the patent system that lets them monopolize for 20 years then let the market crash after.
And complex generics? Yeah those are tough. Inhalers are basically tiny rockets. Getting the particle size right is like nailing a snowflake to a wall. FDA’s new pilot for U.S.-made stuff is smart. We need to stop outsourcing our health to factories with questionable labor practices.
Interesting breakdown. I work in pharma logistics in India and we produce a lot of generic APIs. The quality control is actually very strict here-FDA inspectors come often and they don’t play around. The real issue is the gap between manufacturing standards and distribution. Some countries don’t have good storage, so even a perfect generic can degrade before it reaches the patient. The system works if the chain holds.
Also, Paragraph IV certifications? That’s where the real drama happens. Some companies file them just to delay competitors, not because the patent is invalid. It’s legal but kinda dirty. Still, it’s what keeps prices low long-term.
Wow. So the FDA approves generics based on a 20% margin of error and calls it ‘exact.’ That’s not science. That’s a compromise for lazy regulators and greedy corporations. And you think patients don’t notice? I’ve had people switch to generics and get migraines, nausea, even seizures. They’re not all the same. The FDA knows this. They just don’t care because it saves money. This isn’t healthcare. It’s cost-cutting with a white coat.
You know what’s beautiful? That someone can wake up with diabetes, heart disease, or asthma and still afford their medicine because of this system. It’s not glamorous. No one’s making TikToks about ANDAs. But this is how real change happens-not with slogans, but with paperwork, inspections, and bioequivalence studies.
Don’t let the cynics convince you this is broken. It’s working. It’s saving lives. And if we want to make it better? We don’t tear it down. We fund more reviewers, push for more domestic production, and keep holding the FDA accountable. This system deserves respect.
I just wanted to say thank you for writing this because I used to be scared of generics because I thought they were like fake medicine or something I was being tricked into taking but now I feel so much better knowing that the science is actually really solid and that the FDA doesn’t cut corners even though it’s cheaper and honestly I think more people should know this because I’ve heard so many people say they won’t take generics and I just want them to know it’s not a gamble it’s actually a really smart choice and I hope this helps someone else feel less anxious about their meds
Wait so you’re telling me I can’t even complain about my generic Zoloft making me feel numb because it’s ‘bioequivalent’? What if I’m one of the 1% who reacts to the dye? You think the FDA gives a damn? They’re too busy approving 90 generics a year to care about individual suffering. This isn’t medicine-it’s a supply chain spreadsheet with a stethoscope.