Cardiac Device Eligibility Checker
Check Your Eligibility
Eligibility Results
When the left side of the heart can’t pump blood effectively, everyday activities feel like climbing a mountain. For many who live with left ventricular failure, the promise of a device that steadies the heart’s rhythm or even takes over some of its work can sound like a lifeline. This article breaks down why cardiac device therapy is becoming a core part of treatment plans, what options exist, and how patients can navigate the process from implant to everyday living.
Understanding Left Ventricular Failure
Left Ventricular Failure is a form of heart failure where the left ventricle loses its ability to contract powerfully enough to push blood through the body. The condition typically shows up as shortness of breath, fatigue, and swelling in the legs. According to the Global Heart Institute, about 6 million adults in the United States alone are diagnosed each year, and the prevalence rises sharply after age 60. A key measurement doctors use is the ejection fraction (EF) - the percentage of blood the left ventricle pumps out with each beat. An EF below 35 % usually signals advanced disease and pushes clinicians to consider more aggressive interventions.
What Is Cardiac Device Therapy?
Cardiac Device Therapy refers to a group of implanted technologies that help the failing heart either synchronize its beats, prevent dangerous arrhythmias, or physically assist its pumping function. The three most common devices are Cardiac Resynchronization Therapy (CRT) units, Implantable Cardioverter Defibrillators (ICDs), and Left Ventricular Assist Devices (LVADs). Each addresses a different aspect of the heart’s failure, and many patients end up receiving a combination tailored to their specific needs.
Cardiac Resynchronization Therapy (CRT)
CRT, often called biventricular pacing, delivers tiny electrical pulses to both ventricles so they contract at the same time. In left ventricular failure, the heart’s electrical system can become out of sync, worsening the pump’s efficiency. Studies published in the European Heart Journal in 2023 showed that CRT reduced hospital readmissions by 30 % and improved six‑minute walk distance by an average of 55 meters. The therapy is most effective for patients with a widened QRS complex on ECG, an EF below 35 %, and NYHA Class II‑IV symptoms.
Implantable Cardioverter Defibrillator (ICD)
An ICD monitors the heart’s rhythm continuously and delivers a shock if a life‑threatening ventricular tachycardia or fibrillation episode occurs. While an ICD doesn’t improve pumping directly, it dramatically cuts the risk of sudden cardiac death - a leading cause of mortality in left ventricular failure. The MADIT‑CRT trial reported a 24 % reduction in overall mortality for patients receiving an ICD combined with CRT compared to medication alone.
Left Ventricular Assist Device (LVAD)
LVADs are mechanical pumps that take over part of the left ventricle’s workload. They are typically reserved for patients with end‑stage heart failure who are waiting for a transplant or those who aren’t transplant candidates at all. Modern continuous‑flow LVADs, such as the HeartMate 3, have shown five‑year survival rates above 70 % and a substantial boost in quality‑of‑life scores. Patients often report being able to resume light gardening, short walks, and even some low‑impact sports within months of implantation.
How Device Therapy Improves Outcomes
Across the board, cardiac device therapy targets three major goals: extending life, reducing hospital stays, and lifting everyday energy levels. A 2024 meta‑analysis of 18 randomized trials found that combined CRT‑ICD therapy cut all‑cause mortality by 15 % and cut heart‑failure admissions by nearly one third. LVADs, while more invasive, can turn a terminal prognosis into a manageable chronic condition, allowing patients to live many years beyond what medication alone would permit.
Who Is Eligible? Key Selection Criteria
Eligibility hinges on a mix of clinical measurements and functional assessments. The New York Heart Association (NYHA) classification gauges symptom severity from Class I (no limitation) to Class IV (severe limitation). Most guidelines recommend CRT for NYHA Class II‑IV patients with EF ≤ 35 % and a QRS duration ≥ 130 ms. ICDs are offered to anyone with EF ≤ 35 % after a documented episode of ventricular tachycardia or who meets primary‑prevention risk scores. LVAD candidacy requires EF < 25 % despite optimal medical therapy, plus the ability to manage the device’s external components.
Risks, Maintenance, and Lifestyle Adjustments
No therapy is risk‑free. CRT lead dislodgement, infection at the implant site, and rare device malfunction affect about 5‑7 % of patients. ICD shocks can be painful and may cause anxiety, so many clinicians program the device to deliver anti‑tachycardia pacing first. LVADs demand diligent pump‑controller monitoring, battery changes every few days, and strict sterile technique for driveline care. However, with a robust follow‑up plan and patient education, most complications are manageable and don’t outweigh the benefits.
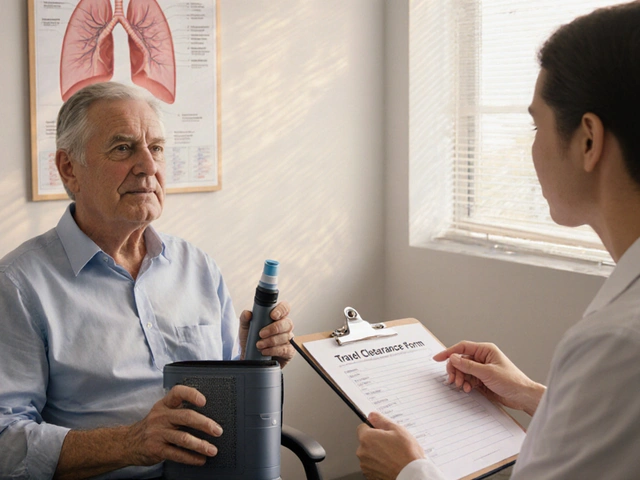
After Implant: What to Expect
Post‑procedure visits usually happen at two weeks, then at three months, and annually thereafter. During these appointments, doctors check device settings, battery life, and heart function via echocardiogram. Patients are encouraged to adopt a heart‑healthy diet, stay active within tolerance, and keep an eye on fluid balance - especially for LVAD users whose pump speed can be adjusted based on activity level. Many support groups exist online and in hospitals, providing peer advice that smooths the adjustment period.
Device Comparison at a Glance
| Feature | CRT | ICD | LVAD |
|---|---|---|---|
| Primary Goal | Resynchronize ventricular contraction | Prevent sudden cardiac death | Assist or replace left‑ventricular pumping |
| Typical Candidates | EF ≤ 35 %, QRS ≥ 130 ms, NYHA II‑IV | EF ≤ 35 % with/without prior arrhythmia | End‑stage HF, EF < 25 %, transplant‑ineligible |
| Survival Benefit | ~15 % reduction in mortality | ~24 % reduction in sudden death | 5‑year survival > 70 % |
| Hospital‑Readmission Impact | -30 % HF admissions | -20 % HF admissions | -40 % admissions (when optimized) |
| Major Risks | Lead dislodgement, infection | Inappropriate shocks, infection | Bleeding, driveline infection, pump thrombosis |
Quick Takeaways
- Cardiac device therapy can extend life and cut hospital stays for left ventricular failure patients.
- CRT improves heart efficiency, ICD stops deadly arrhythmias, and LVAD provides mechanical pump support.
- Eligibility depends on ejection fraction, NYHA class, and ECG/QRS characteristics.
- Risk management and regular follow‑up are crucial for long‑term success.
- Patients often regain meaningful activity levels and better quality of life after implantation.
Frequently Asked Questions
Can cardiac devices cure left ventricular failure?
No. Devices don’t cure the disease, but they can dramatically improve heart function, lessen symptoms, and extend survival when used with medication and lifestyle changes.
How long does an implanted device last?
Most CRT and ICD units have battery lives of 5‑8 years. LVADs can run for many years, but the external pump controller may need periodic replacement.
Will I feel the device while it’s working?
CRT and ICD pacing are usually imperceptible. An ICD shock is felt as a strong jolt, but modern devices aim to avoid shocks when possible. LVAD users hear a low hum from the pump, which many quickly get used to.
What lifestyle changes should I make after implantation?
Follow a low‑sodium diet, maintain a healthy weight, stay active within your limits, and keep up with regular device checks. LVAD patients also need strict driveline hygiene and backup batteries on hand.
Is cardiac device therapy covered by insurance?
In most countries, Medicare, Medicaid, and private insurers cover CRT and ICD for approved indications. LVADs are covered when deemed medically necessary, though prior authorization is common.



When you contemplate the heart as an engine, the notion of synchronizing its rhythm seems almost philosophical, a quest for harmony amidst chaos
the data on CRT and its impact on readmission rates reinforces the idea that technology can act as a mediator between decline and resilience
One must acknowledge, albeit with a certain weary disdain, that the literature often glosses over the nuanced trade‑offs between device invasiveness and marginal survival advantage; the meta‑analysis cited, while impressive on its surface, fails to interrogate the selection bias inherent in trial cohorts, thereby rendering its conclusions somewhat superficial
hey fam i get how scary it can be getting a pump in your chest but trust me the support u feel after a few weeks is real love you can even go back to gardening and feel the sun again keep that hope alive and dont be scared to ask docs any question they vill help u
While the prevailing discourse presents cardiac devices as benign extensions of therapy, a more circumspect examination reveals a lattice of corporate interests and regulatory acquiescence that seldom surfaces in mainstream summaries; one cannot dismiss the possibility that the accelerated approval pipelines are, in part, conduits for undisclosed financial entanglements, thereby inviting a degree of skepticism into any ostensibly altruistic medical narrative
In reflecting upon the comprehensive overview presented, it becomes evident that the integration of cardiac device therapy into the management of left ventricular failure represents a paradigm shift of considerable magnitude, one that demands both clinical acuity and patient-centered advocacy; the nuanced differentiation between CRT, ICD, and LVAD underscores the necessity for individualized assessment based upon ejection fraction, NYHA classification, and electrocardiographic parameters, thereby fostering a tailored therapeutic approach.
Moreover, the empirical evidence delineated-particularly the reduction in hospitalization rates and the augmentation of six‑minute walk distances-substantiates the tangible benefits conferred upon patients, reinforcing the merit of early interdisciplinary consultation.
Simultaneously, the discourse on device-associated risks, such as lead dislodgement, infection, and driveline complications, mandates vigilant postoperative surveillance and patient education, ensuring that the therapeutic gains are not eclipsed by preventable adverse events.
Furthermore, the longitudinal data indicating five‑year survival surpassing 70 percent for LVAD recipients heralds a new horizon wherein end‑stage heart failure transitions from an inexorable decline to a manageable chronic condition, thereby expanding the horizons of survivorship and quality of life.
It is incumbent upon clinicians to adopt a holistic framework that integrates lifestyle modification, dietary considerations, and psychosocial support alongside device implantation, thereby cultivating an environment conducive to optimal outcomes.
This comprehensive approach is bolstered by the availability of support groups and peer mentorship networks, which serve as invaluable resources for navigating the complexities of device maintenance and psychosocial adaptation.
In summation, the synthesis of robust clinical data with patient empowerment strategies delineated within the article furnishes a compelling argument for the broader adoption of cardiac device therapy, inviting ongoing dialogue and collaborative innovation across the cardiology community.
We need to recognize the real-life impact these devices have-patients report regained independence and reduced anxiety, which translates directly into better adherence and overall outcomes; it’s crucial that we continue to push for accessibility and education so no one is left behind