Every year, millions of Medicare beneficiaries get a free, one-on-one review of all their medications. It’s called a Medicare Annual Medication Review, or Comprehensive Medication Review (CMR). But here’s the catch: if you don’t show up prepared, you waste your time-and maybe your health.
Most people think the pharmacist will just look at their prescriptions and say, "Everything looks good." But that’s not how it works. The pharmacist needs to see everything you’re taking-prescriptions, over-the-counter pills, vitamins, herbal teas, even that fish oil you started last winter. If you forget something, or guess a dose, you could miss a dangerous interaction, pay more than you need to, or keep taking a drug that’s no longer helping you.
Here’s the truth: the CMR is only as good as the information you bring. Studies show that when seniors come prepared, satisfaction jumps from 42% to 78%. One woman in Ohio caught a deadly interaction between her blood thinner and a common supplement just by writing down every pill she took. Another man saved $800 a year after his pharmacist spotted a cheaper, equally effective alternative to his cholesterol med.
Who Qualifies for a Medicare Annual Medication Review?
Not everyone gets invited. Medicare Part D plans are required to offer this review, but only to people who meet specific criteria. As of 2025, you’re eligible if you have:
- At least three chronic health conditions (like diabetes, heart disease, COPD, or high blood pressure)
- Take four or more Part D-covered prescription medications (including maintenance drugs)
- Spent at least $1,623 out-of-pocket on covered Part D drugs in the past year
That’s a big change from just a few years ago. In 2023, the cost threshold was over $4,000. Now, more seniors qualify-especially those on multiple generics or who pay for brand-name drugs without insurance help. If you’re unsure, call your Part D plan’s member services. They’ll tell you if you’re targeted for a review this year.
Even if you don’t qualify, ask anyway. Some plans offer reviews to others on a case-by-case basis, especially if you’ve been hospitalized or had a recent change in meds.
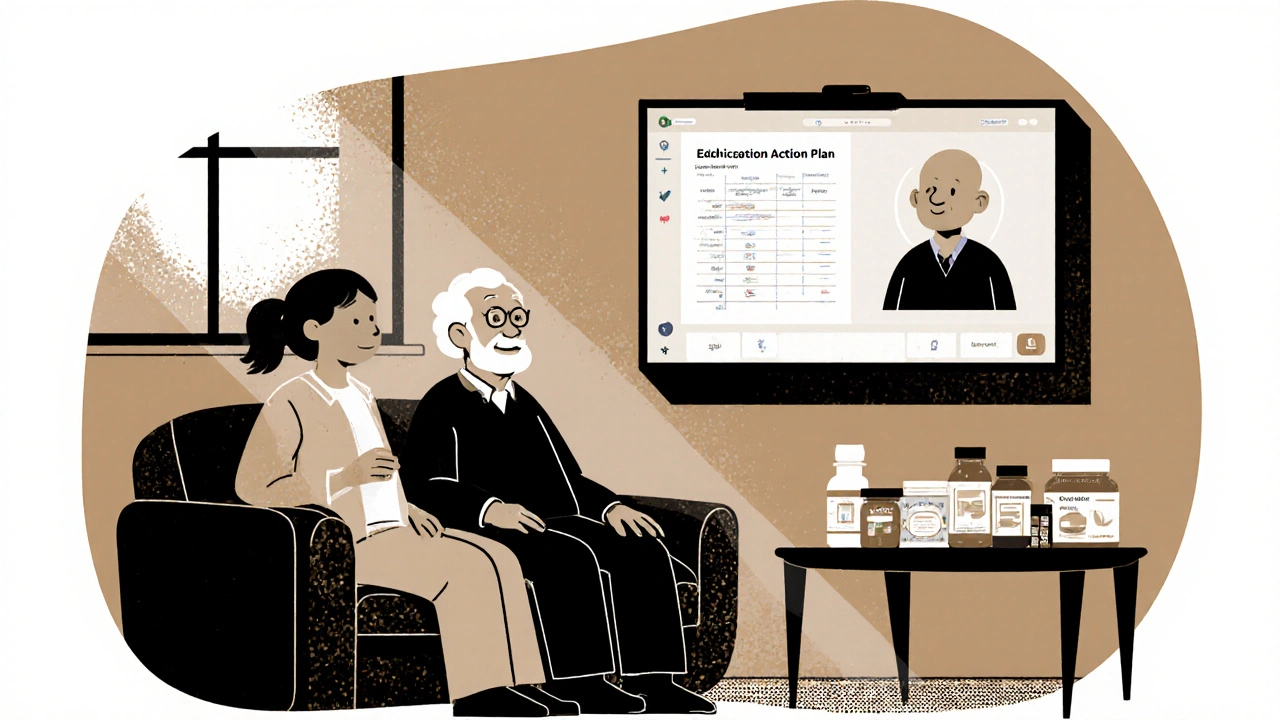
What Happens During the Review?
The CMR isn’t a quick chat at the pharmacy counter. It’s a 30- to 60-minute appointment-usually by phone or video call-with a licensed pharmacist trained in medication therapy management. They’ll go through every single thing you take, including:
- All prescription drugs (even ones from different doctors)
- Over-the-counter meds (pain relievers, sleep aids, antacids)
- Vitamins and supplements (iron, magnesium, melatonin)
- Herbal remedies (ginkgo, garlic pills, turmeric)
- Topical creams or patches (like nicotine or pain patches)
The pharmacist checks for:
- Duplicate prescriptions (two drugs that do the same thing)
- Drug interactions (what happens when meds clash)
- Side effects you haven’t mentioned
- Medications you no longer need
- Cost-saving alternatives
- Adherence problems (like skipping doses because pills are too expensive or confusing)
At the end, you’ll get three documents in the mail:
- Consultation Letter - Summarizes what was discussed
- Medication Action Plan - Lists changes or next steps (like stopping a drug or switching brands)
- Personal Medication List - Your updated, official list to keep and share with all your doctors
This isn’t just paperwork. It’s your personal medication roadmap. Keep it with your other health records. Bring it to every doctor visit.
How to Prepare: The 5-Step Checklist
You can’t wing this. Preparation turns a routine call into a life-changing conversation. Here’s exactly what to do.
Step 1: Gather Every Medication You Take
Don’t rely on memory. Go through every cabinet, purse, nightstand, and medicine drawer. Collect every pill bottle, box, or packet-even the ones you haven’t used in months. You need the original containers, not just a list. Why? Because labels show the exact name, dose, and instructions. A bottle of “ibuprofen” could be 200 mg or 800 mg. The pharmacist needs to see the label.
Pro tip: Take photos of each label with your phone. That way, if you misplace something, you still have the info. You can even use a free app like Medisafe or MyTherapy to snap and store them.
Step 2: Make a Realistic Medication List
Write down:
- Drug name (as it appears on the bottle)
- Dose (e.g., 10 mg, 500 mg)
- How often you take it (once daily, twice a day, as needed)
- Why you take it (e.g., “for blood pressure,” “for arthritis pain”)
- When you started taking it (if you remember)
Include everything-even the stuff you think doesn’t matter. That gummy vitamin with melatonin? The turmeric capsule your daughter gave you? The OTC laxative you use every few weeks? Write it all down. Studies show people forget 2 to 3 medications on average when they just list them from memory.
Use a simple table:
| Medication | Dose | Frequency | Purpose | Started |
|---|---|---|---|---|
| Metformin | 500 mg | Twice daily | Diabetes | Jan 2023 |
| Calcium + D3 | 600 mg / 400 IU | Once daily | Bone health | Mar 2024 |
| Albuterol inhaler | 2 puffs | As needed | Asthma | Oct 2022 |
| Benadryl | 25 mg | At night | Helps me sleep | 2021 |
Step 3: Note Your Concerns
Write down three to five questions or worries. Examples:
- “I feel dizzy after I take my blood pressure pill-should I take it at night instead?”
- “I’ve been forgetting to take my pills. Is there a simpler way?”
- “My cholesterol med costs $120 a month. Is there a cheaper one?”
- “I take six pills at breakfast. Is that too many?”
- “I started taking ginger capsules for joint pain. Is that safe with my blood thinner?”
Don’t hold back. If something feels off, say it. The pharmacist isn’t there to judge-they’re there to fix problems you didn’t even know you had.
Step 4: Bring Recent Health Changes
Did you recently:
- Go to the ER or get hospitalized?
- Start seeing a new doctor?
- Have a fall or change in mobility?
- Notice new symptoms like confusion, fatigue, or swelling?
Bring notes on these-even if they seem unrelated. A change in balance might be caused by a drug interaction. Memory lapses could be from an old antihistamine you’re still taking. Your pharmacist connects the dots between meds and symptoms that your doctor might miss in a 10-minute visit.
Step 5: Bring Someone With You
It’s not just helpful-it’s smart. Bring a family member, friend, or caregiver. You’ll be talking about complex medical info. You might forget something. You might feel overwhelmed. A second set of ears helps. They can also ask questions you didn’t think of.
One man in Florida brought his daughter. She noticed he was taking two different blood thinners-one prescribed by his cardiologist, another by his orthopedist. They’d never told each other. That interaction could have caused internal bleeding.
What to Expect During the Call
The pharmacist will start by confirming your list. They’ll ask:
- “Do you take this every day, or only when you need it?”
- “Have you noticed any side effects?”
- “Do you ever skip doses because of cost?”
- “Do you use a pill organizer?”
They’ll check for red flags:
- Drugs that shouldn’t be taken together (like NSAIDs and blood thinners)
- Medications that lose effectiveness over time
- Drugs that cause drowsiness and increase fall risk
- Overlapping doses (e.g., taking Tylenol and a cold med that also has acetaminophen)
You’ll get clear answers. No jargon. No rushing. They’ll explain what’s working, what’s not, and what to do next.
What If You’re Not Eligible?
If you don’t meet the criteria but still take multiple meds, you still deserve a review. Ask your pharmacist if they offer a free “medication check-up.” Many community pharmacies do. Or ask your doctor for a referral to a medication therapy management program. You can also schedule a Medication Therapy Management session through your Part D plan-even if you’re not automatically targeted.
Some plans now let you request a CMR yourself. Call customer service and say: “I’d like to schedule a Comprehensive Medication Review, even though I’m not on the list.” They can’t refuse if you’re a Part D member.
After the Review: What to Do Next
Don’t just file the documents and forget them.
- Keep your updated Personal Medication List in your wallet or phone.
- Share it with every new doctor, specialist, or hospital you visit.
- Review it every three months. Add new meds. Remove old ones.
- If you get a new prescription, call your pharmacist before filling it. Ask: “Is this safe with what I’m already taking?”
One woman in Arizona kept her list on her fridge. When she fell and went to the ER, the nurses used it to avoid giving her a drug that interacted with her heart med. She credits that list with saving her life.
Common Mistakes to Avoid
Here’s what most people do wrong:
- Bringing only prescriptions - OTC meds and supplements cause half of all dangerous interactions.
- Guessing doses - “I take one of those little white pills.” That’s not enough.
- Not mentioning side effects - “I’m just tired” might mean your meds are too strong.
- Waiting until the last minute - If you wait for the call, you might miss it. Call your plan proactively.
- Thinking it’s not worth it - 87% of seniors who prepared well said the review changed their medication plan for the better.
Don’t be the person who gets rescheduled because they didn’t bring their pill bottles. That’s the #1 complaint on Medicare.gov reviews.
Final Thought: This Is Your Health
The Medicare Annual Medication Review isn’t a bureaucratic formality. It’s your chance to take control. You’re not just a patient-you’re the expert on your own body. You know when something feels off. You know what you can afford. You know what helps you sleep or what makes you dizzy.
This review is designed to listen to you. But only if you speak up.
Take 45 minutes. Gather your meds. Write down your questions. Bring someone you trust. Show up ready. You could prevent a hospital stay, save hundreds of dollars, or even avoid a life-threatening interaction.
That’s not just good healthcare. That’s smart living.
Do I have to pay for a Medicare Annual Medication Review?
No. The Medicare Annual Medication Review (CMR) is a free benefit included with your Medicare Part D plan. There is no copay, deductible, or fee. You do not need to pay anything to receive this service, even if you’re enrolled in a Medicare Advantage plan with Part D coverage.
Can I do the review in person instead of over the phone?
Yes. While many plans offer phone or video consultations, you can request an in-person meeting with a pharmacist at your local pharmacy. Some plans even send a pharmacist to your home if you have mobility issues. When you’re contacted to schedule your review, ask: “Can I meet face-to-face at my pharmacy?” Most will accommodate this request.
What if I don’t want to change my medications?
You’re in charge. The pharmacist will make recommendations, but you don’t have to follow them. If they suggest stopping a drug or switching to a cheaper one, you can say no. However, they’ll explain why they made the suggestion-like risk of side effects or cost savings-and you can discuss alternatives. Your doctor must approve any prescription changes, so the pharmacist will contact them if needed.
How often do I get a Medicare Annual Medication Review?
You’re entitled to one Comprehensive Medication Review every 365 days. If you qualify again next year, you’ll be contacted again. Some plans also offer quarterly Targeted Medication Reviews (TMRs) if you have issues like missed doses or high costs-but those are follow-ups, not full reviews.
What if I forget to prepare and show up without my meds?
You’ll likely be asked to reschedule. Pharmacists need to see your actual pill bottles to verify doses and names. Without them, they can’t safely review your regimen. If you can’t gather everything right away, call your plan back and say: “I need to reschedule-I’ll be ready in a week.” It’s better to wait than to have an incomplete review.
Can my caregiver or family member do the review for me?
No. The review must be conducted with you, the beneficiary, present. However, your caregiver or family member can join you during the call or appointment to help answer questions and take notes. They can’t represent you unless you’ve given them legal authority as a healthcare proxy, which is rare for this service.



Man, I just did my CMR last month and honestly? I didn’t think it’d be worth it. I brought all my bottles, even the expired ones, just to be safe. The pharmacist caught that I was taking two different versions of melatonin-one gummy, one capsule-and I had no idea they both had the same active ingredient. She said I was basically double-dosing myself at night. Now I’m only taking one, and I actually sleep better. Also, she found a cheaper generic for my blood pressure med that saved me $90 a month. I didn’t even know that was possible. Just show up with your stuff. No excuses.
They’re watching us. This is just the beginning. Next they’ll require us to scan our pills with an app and upload our bowel movements to Medicare’s cloud.
From a clinical pharmacotherapy standpoint, the CMR is a critical intervention point in polypharmacy risk mitigation. The pharmacokinetic and pharmacodynamic interactions among CNS depressants, anticoagulants, and OTC supplements like St. John’s wort are under-recognized in geriatric populations. The data supporting reduced hospitalization rates post-CMR is robust, with ORs of 0.63 (95% CI: 0.51–0.78) in recent JAMA studies. This isn’t just paperwork-it’s harm reduction at scale.
OH MY GOODNESS!! I CAN’T BELIEVE PEOPLE ARE STILL IGNORING THIS!! I TOLD MY MOTHER TO BRING HER PILLS LAST YEAR AND SHE SAID, ‘I’LL JUST TELL THEM WHAT I TAKE.’ SHE ALMOST DIED FROM A BLEEDING ULCER BECAUSE SHE WAS TAKING IBUPROFEN WITH HER WARFARIN AND NEVER TOLD ANYONE!! THIS ISN’T A ‘REVIEW’-IT’S A LIFE-SAVING CHECKPOINT!! WHY DO WE LET OUR ELDERLY JUST GUESS THEIR MEDS?!?!
man i just got my cmr last week and wow. i thought i was just gonna sit there and nod while some guy read my pill bottles. but he asked me if i ever felt ‘fuzzy’ after lunch. i said yeah, like a fog. he looked at my list and said ‘you’re taking benadryl for sleep and also that new antihistamine for allergies-both are sedating as hell.’ i had no idea. now i only take one at night and i feel like a new person. also he gave me a sticker that says ‘meds master’ 😎
Why do we let bureaucrats in D.C. decide who gets free health care? I’m on four meds and I pay for everything myself. I don’t get this review because I don’t qualify? That’s not healthcare, that’s class warfare. The government should give this to EVERYONE who’s over 65. Not just the ones who broke the magic dollar threshold. This is ridiculous.
Had my CMR last month. Took me 45 minutes to gather everything. Found out I was taking two different blood pressure meds that did the same thing. Also my pharmacist asked if I’d noticed my legs swelling. I said yeah but thought it was just aging. Turns out it was a side effect of my calcium channel blocker. Switched meds. Swelling gone in a week. No one else asked me that. Not my PCP, not my cardiologist. Just the pharmacist who actually looked at my whole list. This system works if you show up.
It’s funny how we treat medicine like a grocery list-grab what’s on sale, toss in a little turmeric, a pinch of this, a dash of that. But our bodies aren’t soups. They’re ecosystems. And when you throw in unregulated supplements, OTC drugs, and old prescriptions from doctors you haven’t seen in five years? You’re playing Russian roulette with your kidneys, your liver, your brain. The CMR isn’t bureaucracy-it’s a quiet act of rebellion against the idea that we can just ‘wing it’ with our health. I keep my list taped to my fridge. Every morning I look at it. And I say: ‘You’re not just a patient. You’re the CEO of your own body.’
In India, we call this ‘medication reconciliation’-and it’s often done by the family, not just the pharmacist. My mother, who has diabetes and hypertension, always brings her entire medicine box to every doctor visit. We even take photos of labels in case bottles are lost. The concept is simple: trust no one’s memory, not even your own. I’m glad to see the U.S. catching up. This is not a privilege-it is basic dignity in aging. I wish more countries adopted this model. Thank you for sharing this guide-it is a gift to many.
My dad just did this and he’s still talking about it. He said the pharmacist didn’t even look at his phone-he just sat there and asked him how he felt. No rush. No scripts. Just a conversation. Dad said it was the first time anyone ever asked him if he was scared of his meds. That hit me hard. We’re so focused on the pills, we forget the person taking them.
Every single senior I know who skipped this review ended up in the ER within six months. I’ve seen it. I’ve helped clean up the mess. Bring your bottles. Write down your questions. Bring someone. Do it. This isn’t optional. It’s preventative care that saves lives, money, and dignity. Stop making excuses. Your future self will thank you.
My aunt didn’t bring her fish oil. Said it was ‘just a supplement.’ Turns out it was making her blood thin enough to bruise from a sneeze. Pharmacist freaked out. Now she’s on a new regimen. Also, she’s 82 and still takes melatonin gummies like they’re candy. 🍬😴 I told her she’s basically giving her liver a rave party every night. She laughed. Then cried. Then changed her ways. This review saved her from a stroke. I’m telling everyone.
The real issue isn’t the review-it’s the fragmentation of care. My mother sees five different specialists. Each prescribes independently. No one talks to the others. The CMR is the only moment where someone tries to stitch the quilt together. But even then, it’s a one-time event. We need continuous medication management-not an annual checkbox. Still, it’s the best thing we’ve got right now. I print out the Personal Medication List and laminate it. It’s in her purse, her wallet, and taped to the fridge. It’s her lifeline.
I’ve been a community pharmacist for 37 years. I’ve seen everything. People come in with pill bottles from 2009. They say, ‘I think this was for my back?’ I’ve had patients take three different painkillers that all contained acetaminophen and ended up with liver failure. I’ve had grandmas on five antidepressants because three different doctors prescribed them. The CMR isn’t a gimmick. It’s a rescue mission. And if you don’t show up prepared, you’re not just wasting your time-you’re risking your life. I’ve cried helping people realize they were taking something they didn’t need for ten years. Don’t be that person. Bring the bottles.
Look, I’m not a doctor. I’m just a guy who used to take 12 pills a day and thought it was normal. Then I did the CMR. Turns out I didn’t need half of them. My pharmacist said, ‘You’re not sick-you’re overloaded.’ I stopped four meds. Lost 12 pounds. Stopped feeling foggy. Now I take six. And I feel like I’m 55 again. No joke. If you’re on more than five meds? Do this. Even if you think you’re fine. You’re not. You’re just used to feeling like crap. This review? It’s your reset button.