Heartburn Risk Calculator
Recommended Actions
- Take PPIs: 30-60 minutes before meals
- Avoid: lying down within 3 hours of eating
- Medication timing: Antacids at least 1 hour after meals
Heartburn isn’t just a nuisance after a spicy taco night-it’s a sign your digestive system is under stress. For many people, the burning sensation in their chest comes from a mix of what they eat and what they take as medicine. Spicy foods and certain medications don’t just add up-they can team up to make heartburn worse, sometimes dramatically. The good news? You don’t have to give up flavor or skip your meds. You just need to understand how they interact and how to manage them.
Why Spicy Food Triggers Heartburn
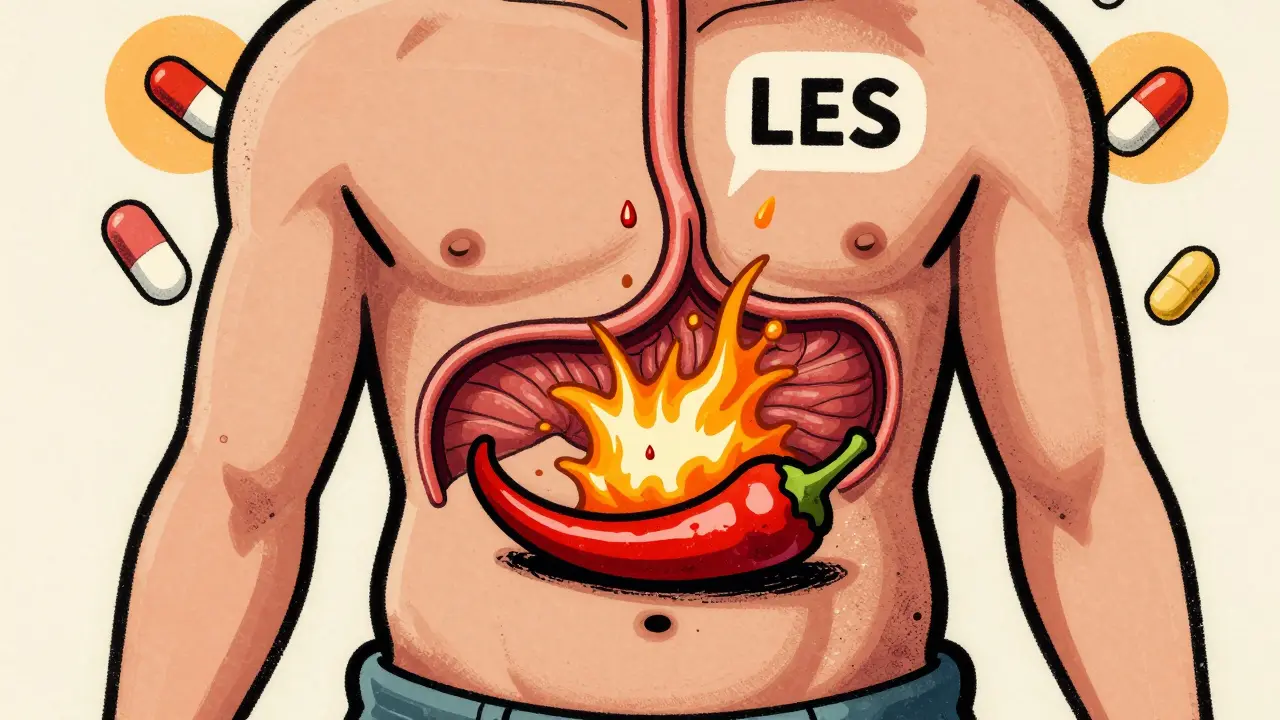
The heat in chili peppers comes from capsaicin, a compound that doesn’t just make your tongue tingle-it also relaxes the lower esophageal sphincter (LES). This muscle is supposed to act like a one-way valve, keeping stomach acid where it belongs. When it loosens, acid creeps up into the esophagus, causing that familiar burn. Studies show capsaicin can reduce LES pressure by 30-40% in sensitive people within 30 minutes of eating.
But here’s the twist: not everyone reacts the same way. A 2023 NIH review found that while some people get heartburn from even mild salsa, others can eat hot wings with no issues. Individual sensitivity to capsaicin varies from 10 to 100 mg per meal. That means your trigger point might be completely different from your friend’s. The key isn’t avoiding spice universally-it’s finding your personal threshold.
Medications That Make Heartburn Worse
Many common prescriptions and over-the-counter drugs quietly sabotage your digestive system. Aspirin and ibuprofen, for example, don’t just relieve pain-they can irritate the lining of your esophagus and stomach. Regular use increases your risk of erosive esophagitis by 15-30%, according to FDA reports.
Beta blockers, often prescribed for high blood pressure, are another hidden culprit. The Framingham Heart Study update from 2023 showed a 22% higher chance of GERD symptoms in users. Anticholinergics-used for motion sickness or overactive bladder-relax the LES in 68% of people who take them. Even asthma meds like theophylline and heart meds like nitrates can drop LES pressure by 28-45%.
And then there’s the class of drugs most people think helps: antacids. While they give quick relief, using them more than two or three times a week can backfire. Aluminum-based antacids can block absorption of antibiotics like tetracycline by half and fluoroquinolones by up to 90%. That’s not just inconvenient-it can make your infection worse.
How Medications Like Pantoprazole Lose Effectiveness
If you’re taking pantoprazole (or another proton pump inhibitor) to control acid, you might be wondering why it’s not working as well as it used to. The answer? What you’re eating. Spicy foods, fatty meals, coffee, chocolate, and alcohol all reduce how well your body absorbs these drugs. Pharmacokinetic studies show absorption drops by 18-23% when taken within two hours of these triggers.
Pantoprazole needs to be taken 30-60 minutes before your first meal to work properly. If you’re eating a spicy lunch at noon and taking your pill at 11:30 a.m., but then have a cup of coffee at 12:30 p.m., you’re undoing half the benefit. The drug isn’t failing-you’re giving it a hard time.
And it’s not just about timing. User reviews on Drugs.com show 34% of people on pantoprazole report reduced effectiveness when they eat spicy foods. This isn’t placebo-it’s chemistry.

What Actually Works: A Realistic Plan
Forget the idea that you must choose between spicy food and peace of mind. The most effective strategy combines smart timing, personal testing, and medication discipline.
Step 1: Track your triggers
Keep a simple food and symptom diary for two weeks. Write down everything you eat, what meds you take, and when heartburn hits. Look for patterns. Maybe it’s not the salsa-it’s the salsa with your evening ibuprofen. Or maybe it’s the coffee after your pantoprazole.
Step 2: Test one thing at a time
Try eliminating the top two suspected triggers for 7-10 days. Then add them back one at a time. Did your heartburn return when you had hot sauce? Or was it the wine you drank with it? This method, used in clinical practices, works for 82% of people within two weeks.
Step 3: Time your meds right
Take PPIs like pantoprazole 30-60 minutes before breakfast. Take antacids like Tums or Rolaids at least one hour after meals, or at bedtime. Never take antacids within four hours of other medications-they interfere with absorption. This simple shift can make a huge difference.
Step 4: Avoid lying down
Wait at least three hours after eating before lying down. Gravity helps keep acid in your stomach. Studies show this reduces nighttime reflux by 60%. Elevating the head of your bed by 6-8 inches adds another layer of protection.
The Bigger Picture: Why Personalization Matters
Doctors used to tell everyone with GERD to avoid spicy food, caffeine, and chocolate. But newer guidelines from the American Gastroenterological Association (June 2023) say that’s outdated. There’s no strong evidence that spicy food causes GERD in everyone. What matters is what triggers your symptoms.
Research presented at the 2023 Digestive Disease Week conference showed that with a 12-week gradual exposure plan, 65% of people could safely reintroduce spicy foods without flare-ups. This isn’t about fear-it’s about building tolerance.
Meanwhile, the market is shifting. The $12.5 billion U.S. GERD drug market is slowing because long-term PPI use carries risks-kidney problems, nutrient loss, even possible heart issues. Meanwhile, personalized nutrition and lifestyle approaches are growing at 8.3% a year. Hospitals are now hiring dietitians to run GERD programs, and those patients see 33% better outcomes and 27% lower medication costs.

When to Be Concerned
Heartburn that comes and goes is one thing. But if you’re relying on antacids every day, or if your symptoms are getting worse despite changes, it’s time to dig deeper. Masking symptoms with medication can hide serious conditions like hiatal hernias, Barrett’s esophagus, or even early signs of esophageal cancer.
Red flags include: trouble swallowing, unexplained weight loss, vomiting blood, or black, tarry stools. These aren’t normal. Don’t wait. Get checked.
Final Takeaway: You Have More Control Than You Think
You don’t have to live with constant heartburn. You also don’t have to give up your favorite meals forever. The solution isn’t extreme restriction-it’s smart adjustments. Test your triggers. Time your meds. Listen to your body. Most people find their balance within weeks. And when you do, you’re not just avoiding pain-you’re taking back control of your health.



Spicy food + ibuprofen = my Saturday night special 😈 I used to think I was just "bad at digestion" until I tracked it. Now I take my Advil in the morning, save the ghost pepper wings for Sunday brunch, and life’s a dream. Also, coffee after pantoprazole? Big mistake. I learned that the hard way. 🤫☕️
They don’t want you to know this, but antacids are a trap. They’re the opioid of heartburn-quick fix, long-term decay. Your stomach needs acid. You’re not broken. The system is.
Okay but real talk-what if you’re just one of those people who can eat 5 ghost peppers and still sleep like a baby? 🤷♀️ I’ve never had heartburn in my life. Maybe the real issue is we’re all being told to fear food instead of listening to our bodies. I eat hot sauce with everything. No problems. Maybe it’s not the spice-it’s the anxiety around it?
America’s getting soft. Back in my day, we ate hot wings, took aspirin, and didn’t whine about heartburn. Stop treating your stomach like a glass vase.
Interesting how the article conveniently omits the fact that Big Pharma profits from people believing they’re "broken" and need lifelong PPIs. You’re not supposed to know that GERD is often caused by low stomach acid, not too much. They sell you drugs to suppress symptoms, not fix the root cause. And yes, I’ve read the studies. All of them.
Also, the NIH review? Sponsored by a PPI manufacturer. Check the funding. The system is rigged.
Just wanted to add-timing your PPI before breakfast is huge. I used to take mine at night and wondered why it didn’t work. Switched to 45 min before my first meal, cut my antacid use by 80%. Also, elevating your bed? Game changer. I used two bricks under the legs. No joke. It’s dumb, but it works.
One must question the underlying epistemological framework of this "personalized nutrition" narrative. It is a neoliberal construct, designed to individualize systemic health failures. The real culprit? Industrialized food systems, agrochemical-laden chili crops, and pharmaceutical lobbying. The NIH study? A performative gesture masking corporate capture. The 8.3% growth in personalized nutrition? A distraction from the true pathology: capital’s colonization of the body.
OMG I KNEW IT!! I told my doctor last week that my heartburn got worse after I started eating Indian food with my blood pressure meds-and she laughed at me. LOL. But guess what? I stopped taking my beta blocker after dinner and now I eat vindaloo every Friday. No burning. No pills. I’m basically a genius. Also, I think the government is putting fluoride in the chili powder to make us dependent on antacids. Wake up, sheeple. 🌶️👁️
Hey everyone-just wanted to say this post saved my life. I was on PPIs for 3 years. Felt like a zombie. Started tracking like Jake said-turned out it was coffee 30 mins after my pill. One change. One week. No more burning. I’m not saying you have to be perfect. Just be curious. Your body’s trying to tell you something. Listen. You’ve got this. 🙌