Antibiotic Selection Decision Tree
This tool helps determine whether levofloxacin or an alternative antibiotic is more appropriate based on patient factors and infection type.
Quick Take
- Levofloxacin is a broad‑spectrum fluoroquinolone often used for respiratory and urinary infections.
- Common alternatives include ciprofloxacin, moxifloxacin, amoxicillin, doxycycline, and trimethoprim‑sulfamethoxazole.
- Choose levofloxacin when you need once‑daily dosing and strong activity against Gram‑negative bugs.
- Pick alternatives if you’re worried about fluoroquinolone‑related tendon risks or FDA warnings.
- Consider cost, local resistance patterns, and patient comorbidities before deciding.
Levofloxacin is a synthetic, broad‑spectrum fluoroquinolone antibiotic that interferes with bacterial DNA gyrase and topoisomerase IV, halting DNA replication. It was approved in the United States in 1996 and quickly became a go‑to option for community‑acquired pneumonia, acute bacterial sinusitis, and uncomplicated urinary tract infections. Levofloxacin offers the convenience of once‑daily dosing and excellent oral bioavailability, which means you can switch from IV to pills without losing efficacy.
While levofloxacin packs a punch, it belongs to the fluoroquinolone class, a group that has attracted scrutiny over the past decade. The U.S. FDA issued several boxed warnings highlighting risks such as tendon rupture, peripheral neuropathy, and potentially serious mental health effects. These safety concerns push clinicians and patients alike to weigh alternatives carefully.
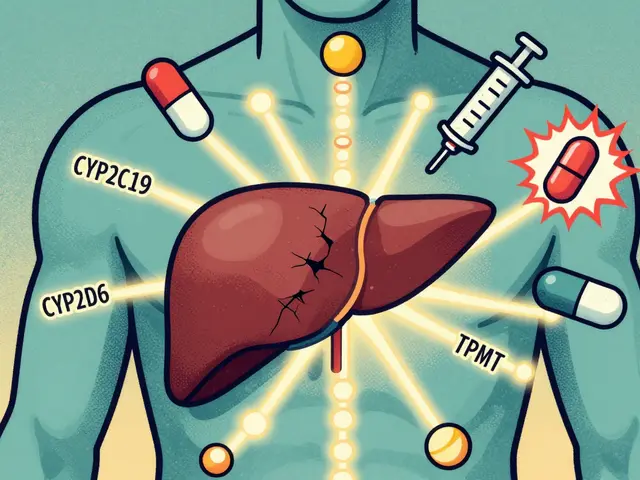
How Fluoroquinolones Work
Fluoroquinolones, including levofloxacin, target bacterial enzymes essential for DNA processes. By binding to DNA gyrase (in Gram‑negative bacteria) and topoisomerase IV (in Gram‑positive bacteria), they prevent the supercoiling and uncoiling of DNA strands, a step needed for replication. This dual‑target action gives them a broad antibacterial range but also raises the bar for bacterial resistance. When resistance emerges, it often involves mutations in the target enzymes or efflux pump overexpression.
Key Alternatives Overview
Below are the most frequently considered substitutes, each with its own strengths and drawbacks.
Ciprofloxacin is another fluoroquinolone, slightly older than levofloxacin, with a stronger focus on Gram‑negative coverage, especially for urinary tract infections and certain types of gastroenteritis.
Moxifloxacin is a newer fluoroquinolone that leans toward enhanced activity against atypical respiratory pathogens, making it a solid choice for community‑acquired pneumonia when resistant organisms are suspected.
Amoxicillin belongs to the beta‑lactam family. It is a narrow‑spectrum penicillin that works well for many ear, nose, and throat infections, as well as uncomplicated pneumonia caused by susceptible Streptococcus pneumoniae.
Doxycycline is a tetracycline antibiotic offering a broad spectrum that includes atypical organisms like Mycoplasma and Chlamydia. It’s also useful for tick‑borne diseases and certain skin infections.
Trimethoprim‑sulfamethoxazole (TMP‑SMX) combines two agents to block folic acid synthesis in bacteria, providing reliable coverage for urinary tract infections, some skin infections, and certain pneumocystis prophylaxis.
Side‑Effect Profiles at a Glance
All antibiotics have potential adverse events, but the patterns differ.
- Levofloxacin: Tendonitis/tendon rupture (especially in older adults), QT‑prolongation, photosensitivity, CNS effects (e.g., anxiety, insomnia).
- Ciprofloxacin: Similar tendon risks, plus higher likelihood of gastrointestinal upset and possible drug‑drug interactions with antacids.
- Moxifloxacin: Greater QT‑prolongation risk, hepatic enzyme elevation.
- Amoxicillin: Generally mild GI upset, rare allergic reactions.
- Doxycycline: Photosensitivity, esophageal irritation, possible candidiasis.
- TMP‑SMX: Stevens‑Johnson syndrome (rare), hyperkalemia, renal function impact.

Cost and Convenience Comparison
| Antibiotic | Spectrum | Typical Indications | Common Side Effects | Dosing Frequency | Average Monthly Cost (USD) |
|---|---|---|---|---|---|
| Levofloxacin | Broad (Gram‑+, Gram‑‑) | Respiratory, urinary, skin infections | Tendon pain, QT prolongation, CNS effects | Once daily | $25‑$45 |
| Ciprofloxacin | Strong Gram‑‑, moderate Gram‑+ | UTIs, gastroenteritis | GI upset, tendon issues | Twice daily | $15‑$30 |
| Moxifloxacin | Broad, excellent for atypicals | Pneumonia, sinusitis | QT prolongation, liver enzyme rise | Once daily | $35‑$55 |
| Amoxicillin | Narrow (mainly Gram‑+) | EAR infections, uncomplicated pneumonia | Allergic rash, mild GI upset | Three times daily (or BID extended‑release) | $5‑$12 |
| Doxycycline | Broad, covers atypicals | Tick‑borne diseases, acne, atypical pneumonia | Photosensitivity, esophageal irritation | Once or twice daily | $10‑$20 |
| TMP‑SMX | Broad, especially urinary pathogens | UTIs, skin infections, PCP prophylaxis | Rash, hyperkalemia, renal impact | Twice daily | $8‑$18 |
When Levofloxacin Makes Sense
If you need a single pill that covers a wide range of bacteria and you value simplicity, levofloxacin is hard to beat. Its 99% oral bioavailability means you can start IV in the hospital and switch to a tablet for the rest of the course without a dose adjustment. For patients who struggle with multiple daily doses-think elderly patients with arthritis-once‑daily dosing improves adherence.
Additionally, levofloxacin’s potency against certain resistant Gram‑negative organisms (e.g., Pseudomonas aeruginosa) can be a lifesaver when culture data are pending, provided local antibiograms show susceptibility.
When to Pick an Alternative
Safety concerns are the biggest driver to switch away from levofloxacin. Patients over 60, those on chronic steroids, or individuals with a history of tendon problems should avoid fluoroquinolones when possible. For pregnant or breastfeeding women, beta‑lactams like amoxicillin or tetracyclines (except doxycycline, which is contraindicated in pregnancy) are preferred.
Local resistance patterns also play a role. In regions where fluoroquinolone resistance among Escherichia coli exceeds 20%, agents like TMP‑SMX or amoxicillin‑clavulanate often provide better first‑line coverage for uncomplicated UTIs.
Practical Tips for Prescribing
- Confirm the infection site and likely pathogens before reaching for a broad agent.
- Check the patient’s medication list for potential interactions (e.g., antacids, warfarin, theophylline).
- Assess kidney function; levofloxacin is renally cleared, and dose adjustment is needed for CrCl < 50mL/min.
- Discuss tendon‑related warning signs-sudden heel or shoulder pain-so patients know when to stop and call their doctor.
- Document the rationale for choosing a fluoroquinolone in the chart to satisfy antimicrobial stewardship audits.
Bottom Line Decision Tree
Use the flow below to narrow your choice quickly:
- Is the patient >60years old OR on chronic steroids? → Consider non‑fluoroquinolone.
- Is the infection a suspected Pseudomonas infection? → Levofloxacin or ciprofloxacin (if susceptible).
- Is the organism a typical respiratory pathogen (Streptococcus, Haemophilus) with low resistance? → Amoxicillin or doxycycline may suffice.
- Is cost a major barrier? → Amoxicillin or TMP‑SMX are cheapest options.
- Do you need once‑daily dosing for adherence? → Levofloxacin or moxifloxacin.

Frequently Asked Questions
Can I take levofloxacin if I have a tendon injury?
No. The FDA specifically warns against using fluoroquinolones, including levofloxacin, in anyone with a recent tendon injury or a history of tendon rupture. The drug can weaken connective tissue and increase the risk of a repeat injury.
Is levofloxacin safe for pregnant women?
Levofloxacin is classified as pregnancy category C, meaning risk cannot be ruled out. Safer alternatives like amoxicillin or erythromycin are generally recommended unless no other options are viable.
What makes moxifloxacin different from levofloxacin?
Moxifloxacin has stronger activity against atypical respiratory organisms (e.g., Mycoplasma, Chlamydia) and a slightly higher risk of QT‑interval prolongation. Levofloxacin, on the other hand, offers broader Gram‑negative coverage and is often cheaper.
How do I know if my bacterial infection is resistant to levofloxacin?
The best way is to order a culture and sensitivity test. In the meantime, look at local antibiograms-many health districts publish resistance rates for common pathogens. If resistance exceeds 20‑30% for the likely bug, pick another agent.
Is once‑daily dosing really better for adherence?
Studies show patients are about 30% more likely to complete a 5‑day course when they only have to remember one dose a day. Levofloxacin’s pharmacokinetics make it a strong candidate for that simplicity.


When you’re weighing levofloxacin against its peers, start with the infection site because that drives the spectrum you need. For community‑acquired pneumonia, levofloxacin’s once‑daily dosing and high oral bioavailability make it a convenient bridge from IV to pill. In urinary tract infections, its gram‑negative potency is useful, but remember local E. coli resistance rates often exceed 20 %, so culture data are essential. The drug’s safety profile demands attention: patients over 60, those on chronic steroids, or anyone with a history of tendon disorders should be steered toward non‑fluoroquinolones. Tendon rupture risk, although rare, is amplified by concurrent corticosteroid use, and the FDA’s boxed warning is not to be taken lightly. QT‑prolongation is another cardiac concern; obtain a baseline ECG if the patient has known arrhythmias or is on other QT‑extending meds. Renal clearance means you must dose‑adjust for creatinine clearance below 50 mL/min, otherwise drug accumulation can occur. If you need broad coverage for atypical organisms like Mycoplasma or Chlamydophila, moxifloxacin edges out levofloxacin with superior activity. Cost is a practical barrier for many; generic levofloxacin sits around $25‑$45 per month, while amoxicillin or doxycycline can be under $15. Adherence improves dramatically with once‑daily regimens, so for patients who struggle with multiple doses, levofloxacin remains attractive. Nevertheless, in regions with high fluoroquinolone resistance, trimethoprim‑sulfamethoxazole or amoxicillin‑clavulanate often provide better first‑line coverage for uncomplicated UTIs. Always document the rationale for choosing a fluoroquinolone in the medical record to satisfy antimicrobial stewardship audits. For pregnant patients, avoid levofloxacin altogether; beta‑lactams are the safer class. Finally, educate patients on warning signs such as sudden shoulder or Achilles pain and instruct them to discontinue the drug and seek care immediately.
Honestly this levofloxacin hype is overblown its risks outweigh any convenience you think you get
Take a look at the QT issue – if you’re already on anti‑arrhythmics, adding levofloxacin can push you into dangerous territory. Consider a beta‑lactam instead.
True, the cardiac side effect is real, but for a short 5‑day course the absolute risk stays low. Still, I always run an ECG when the patient has a borderline QT.
Avoid levofloxacin if you have tendon pain.
From a cultural standpoint, many patients in low‑resource settings prefer the cheapest effective option. Amoxicillin and doxycycline are often more accessible, and their side‑effect profiles are generally milder.
Accessibility matters, yet the decision tree in the post already flags cost as a key factor – it’s a good reminder to check local formulary prices before defaulting to levofloxacin.
When you consider drug‑drug interactions, levofloxacin can chelate with antacids and iron supplements, dropping its serum levels significantly. Advise patients to separate dosing by at least two hours.
Good point – timing is crucial. Also, watch out for warfarin; levofloxacin may enhance its anticoagulant effect.
For someone who can’t remember multiple doses a day, levofloxacin’s once‑daily schedule is a real win.
Agreed, adherence improves, but we must balance that with the safety warnings – especially in the elderly.
From a dramatic perspective, the stakes feel high – a single misstep with a fluoroquinolone can lead to a lawsuit. That’s why many clinicians now prefer narrower‑spectrum agents when culture data support them.
I hear you; the legal risk adds pressure. Still, when the pathogen is unknown and the patient is septic, broad coverage can be life‑saving.
Levofloxacin is overprescribed; cut it out of your protocol unless absolutely necessary.
Balance efficacy, safety, and cost for each patient.