Statin Symptom Tracker
Statin Symptom Tracker
Based on the SAMSON study, 90% of symptoms people attribute to statins are actually due to the nocebo effect. Track your symptoms to determine if your pain is caused by the drug or your expectations.
Log Your Symptoms
Symptom Trends
Your symptom data will appear here as you log entries. Look for patterns showing symptoms that occur consistently across all conditions (likely nocebo) or symptoms that only appear with statins (possible real side effect).
More than half the people who stop taking statins do so because they think the pills are giving them muscle pain. But what if the pain isn’t from the drug at all? What if it’s from expectation?
What You’ve Been Told vs. What Actually Happens
You’ve probably heard the warning: statins can cause muscle aches, fatigue, even serious damage. It’s printed on the bottle, repeated in doctor’s offices, and amplified online. So when you start taking one and feel a twinge in your thigh, it’s natural to blame the pill. But here’s the twist: in a landmark 2021 study called SAMSON, researchers gave people who had quit statins due to side effects three types of pills over 12 months-real statins, sugar pills, and nothing at all. And guess what? The muscle pain didn’t care which pill they took. It showed up just as often with the sugar pill as with the real drug. The numbers don’t lie. When patients took the placebo, their pain score averaged 15.4 out of 100. When they took the statin? 16.3. The difference? Statistically meaningless. Meanwhile, on the days they took nothing, pain dropped to just 8.0. That means 90% of the symptoms people blamed on statins were actually happening whether the pill had any active ingredient or not. This isn’t imagination. It’s biology. Your brain, wired by fear, is triggering real physical sensations.The Science Behind the Nocebo Effect
The nocebo effect is the dark twin of the placebo effect. Placebo: you feel better because you believe a treatment works. Nocebo: you feel worse because you believe it will hurt you. It’s not weak-mindedness. It’s real neurobiology. Stress hormones spike. Pain pathways light up. Muscles tense. Your body responds to what your mind expects-whether that expectation is true or not. In statin trials, this effect is unusually strong. Why? Because statins are one of the most talked-about drugs on the planet. Millions read about side effects before even filling their prescription. A 2022 study found that people who read about muscle pain from statins were twice as likely to report it later-even if they were on a sugar pill. The more you know about the risk, the more likely you are to feel it. This doesn’t happen with every drug. Compare statins to blood pressure meds or antidepressants. In blinded trials, people on placebo report far fewer side effects than those on statins. Why? Because statins come with a unique storm of public messaging, fear-based marketing, and anecdotal horror stories online. The drug itself? It’s incredibly safe. The risk of serious muscle damage? Less than one in a million. The risk of feeling pain because you expect it? Much, much higher.Why Doctors Missed This for So Long
For years, doctors assumed that if a patient felt pain after starting a statin, the drug was the cause. They’d switch brands, lower the dose, or stop it altogether. But blinded trials-where neither patient nor doctor knows who’s getting the real drug-showed no difference in muscle pain between statin and placebo groups. The problem? Those trials rarely asked patients to track daily symptoms. They relied on vague checklists at 3-month visits. That’s like judging your mood by asking, “How are you feeling?” once a year. The SAMSON trial changed that. Instead of asking patients to recall pain after weeks, they used a smartphone app to rate symptoms every day. The result? A clear pattern: pain spiked within days of starting any pill-even the sugar one-and faded just as fast when they stopped. That’s not how real drug toxicity works. Real side effects don’t vanish overnight. They linger. They build. This pattern-fast on, fast off-was the smoking gun. It wasn’t the statin. It was the expectation.
What This Means for You
If you’ve stopped your statin because of muscle pain, you’re not alone. And you’re not weak. But you might have been misled. The good news? Most people who thought they were intolerant can go back on statins-once they understand what’s really happening. In the SAMSON trial, half the patients who completed the study restarted statins after seeing their own data. One man in his 70s had stopped three different statins over five years. After seeing his symptom scores matched perfectly between statin and placebo, he restarted rosuvastatin at 5mg. Within a month, his LDL dropped from 142 to 68. No pain. No problem. You don’t need fancy tech to try this. Ask your doctor for a simple 3-month trial: one month on statin, one month on placebo, one month off. Track your symptoms daily on a scale of 0-10. You’ll likely see the same pattern: pain on statin? Check. Pain on placebo? Check. Pain off everything? Much lower. That’s not coincidence. That’s proof.What About Real Side Effects?
This isn’t about dismissing pain. It’s about distinguishing real danger from false alarms. True statin-induced muscle damage-rhabdomyolysis-is extremely rare. Less than one case per million users. It comes with dark urine, extreme weakness, and sky-high enzyme levels. If you have those, stop the drug and get tested. But if you just feel a dull ache in your legs after a long day? That’s probably not your statin. That’s your brain. Some patients do have true intolerance. But they’re the exception. For the vast majority, the problem isn’t the drug. It’s the story they’ve been told. And stories can be rewritten.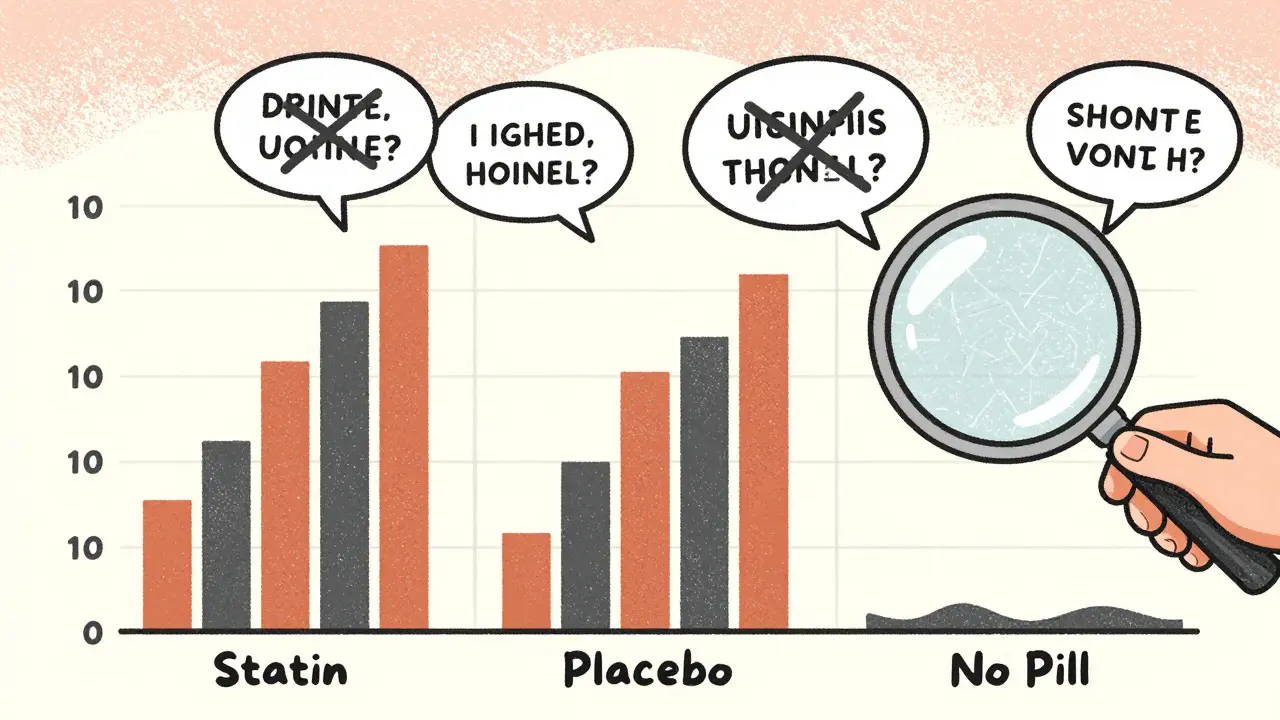
How to Get Back on Statins-The Smart Way
If you’ve quit statins and want to try again, here’s how to do it without falling into the same trap:- Start low: Use 5mg of rosuvastatin or 10mg of atorvastatin. You don’t need a high dose to get benefits.
- Track daily: Use a free app or paper journal. Rate muscle pain, fatigue, and other symptoms from 0-10 each day.
- Use a placebo control: Ask your doctor for placebo pills (sugar pills) to take for a month. Compare how you feel on statin vs. placebo vs. nothing.
- Don’t read side effect lists before starting. If you’ve already read them, forget them. Focus on your own data, not online horror stories.
- Give it time: Symptoms from nocebo usually peak in the first week and fade. Real side effects get worse.
The Bigger Picture
Every year, millions of people stop statins because they think they can’t tolerate them. That’s not just a personal loss-it’s a public health crisis. Statins prevent heart attacks and strokes. But if you stop taking them, your risk goes up. The cost of this non-adherence? Over $11 billion a year in preventable heart events in the U.S. alone. Cardiologists are finally catching on. In 2020, only 22% of lipid specialists talked to patients about the nocebo effect. By 2023, that number jumped to 68%. Hospitals are training staff. Apps are being built to track symptoms. Even pharmaceutical companies are changing their patient materials to explain this phenomenon. This isn’t about blaming patients. It’s about giving them back control. When you understand that your pain might be a trick of the mind, you’re not powerless. You’re equipped. You can test it. You can prove it to yourself. And if the numbers show it’s not the drug, you can get back on the one thing proven to save your life.What to Do Next
If you’re on a statin and worried about side effects: track your symptoms for 30 days. Don’t assume anything. Just record. If you quit statins because of pain: ask your doctor about a structured rechallenge. Bring the SAMSON study. Ask for placebo pills. Ask for a symptom tracker. If you’re a doctor: stop saying, “It’s probably just the statin.” Say, “Let’s find out together.” The truth is simple: statins are one of the safest, most effective drugs ever made. The biggest threat isn’t the pill. It’s the fear around it.Can the nocebo effect cause real muscle damage?
No. The nocebo effect causes symptoms like pain, fatigue, or stiffness-but it does not cause actual muscle tissue damage or elevated CPK enzymes. True statin-induced myopathy or rhabdomyolysis is biochemical and requires lab testing. If your CPK levels are high and you have severe weakness or dark urine, that’s a medical emergency, not a nocebo response.
Is it possible to have both a nocebo effect and real statin side effects?
Yes, but they’re rare together. Most people who think they have statin intolerance are experiencing the nocebo effect. A very small percentage (less than 1%) have true pharmacological sensitivity. The key is testing: if symptoms disappear on placebo and return only on statin, then it’s likely real. But if symptoms are identical on both, it’s nocebo. Tracking symptoms over time is the only way to tell.
Why do statins have such a strong nocebo effect compared to other drugs?
Statins are widely prescribed, heavily marketed, and surrounded by public fear. Side effects are loudly discussed in media, patient forums, and even on pill bottles. Unlike many drugs, statins are taken by healthy people to prevent future disease-so any discomfort feels like a betrayal. This combination of high visibility, widespread use, and preventative purpose makes statins uniquely vulnerable to the nocebo effect.
Can I restart statins after quitting for years?
Absolutely. Many people who quit statins years ago successfully restart them after understanding the nocebo effect. Studies show that over half of patients who previously stopped due to side effects can tolerate statins again when given clear, personalized data showing their symptoms weren’t caused by the drug. Starting with a low dose and tracking symptoms daily greatly increases success.
Do I need blood tests to know if my pain is from the nocebo effect?
Not necessarily. Blood tests like CPK only detect real muscle damage, which is extremely rare. If your CPK is normal and your pain matches the pattern of the nocebo effect-peaking quickly after starting any pill and fading when you stop-then the evidence points to expectation, not toxicity. Symptom tracking over time is more useful than a single blood test for diagnosing nocebo.
Are there apps or tools to help track statin symptoms?
Yes. Apple Health and Google Fit now partner with medical centers to offer statin symptom trackers. You can also use free apps like Symple or even a simple spreadsheet. The goal is daily logging: rate pain, fatigue, and other symptoms on a scale of 0-10. After a month, compare how you felt on statin, placebo, and no-pill days. The pattern will tell you the truth.



Bro, I used to swear statins wrecked my legs-until I did the placebo thing. Turned out my pain was worse on days I *thought* I took the statin. Mind blown. I’m back on 5mg rosuvastatin and my LDL’s at 62. No pain. Just peace. 🙌
This is a remarkably well-documented and clinically significant observation. The SAMSON trial methodology is robust, and the implications for patient education are profound. It underscores the necessity of integrating behavioral neuroscience into routine cardiovascular care.
I’ve been a primary care doc for 18 years, and I used to write off patient complaints as ‘just psychosomatic.’ Not anymore. This isn’t in their head-it’s in their nervous system. The brain’s expectation triggers real physiological responses: cortisol spikes, muscle tension, pain signaling. It’s not weakness. It’s biology. We need to stop shaming patients and start giving them tools-like daily symptom logs and placebo trials. I’ve had 12 patients restart statins after this approach. Eleven are still on them six months later. That’s not magic. That’s science.
And yes, if you’re reading this and you quit statins because of ‘muscle pain,’ you’re not crazy. You’re just caught in a feedback loop of fear. But here’s the good news: you can break it. Track your symptoms. Use a free app. Compare days you take the pill vs. days you don’t. You might be shocked. I’ve seen it too many times.
Also, stop Googling side effects before you start. Seriously. The internet is a minefield of anecdotal horror stories. Your doctor’s office isn’t. Your own data is.
And if you’re a clinician: stop saying ‘it’s probably the statin.’ Say ‘let’s test it together.’ That’s how you rebuild trust.
statins r for sheep. u think ur smart cuz u read a study? lol. my uncle died from statin myopathy. u dont know sh*t.
I tried this and it worked but my doctor laughed at me when I asked for placebo pills like some kind of hippie. I tracked my pain for 30 days and the pattern was insane. Same pain on sugar pill. Same pain on statin. Zero pain when I skipped. I showed him the data. He still said 'it's probably just anxiety.' Well guess what I'm not taking it again and my heart is fine thanks.
so you're saying the pharmaceutical companies are lying to us again? and doctors are in on it? i knew it. they want us dependent. this is all a scam to keep us buying pills. i'm going raw vegan and doing cold plunges instead. #noceboisacult