When you take omeprazole and clopidogrel together, something subtle but powerful happens in your liver. It’s not a side effect you can feel - no nausea, no dizziness. But it can weaken clopidogrel’s ability to protect your heart. This isn’t theoretical. It’s backed by years of research, FDA warnings, and real-world outcomes. And if you’re on both drugs, you need to know exactly what’s going on.
How Clopidogrel Actually Works
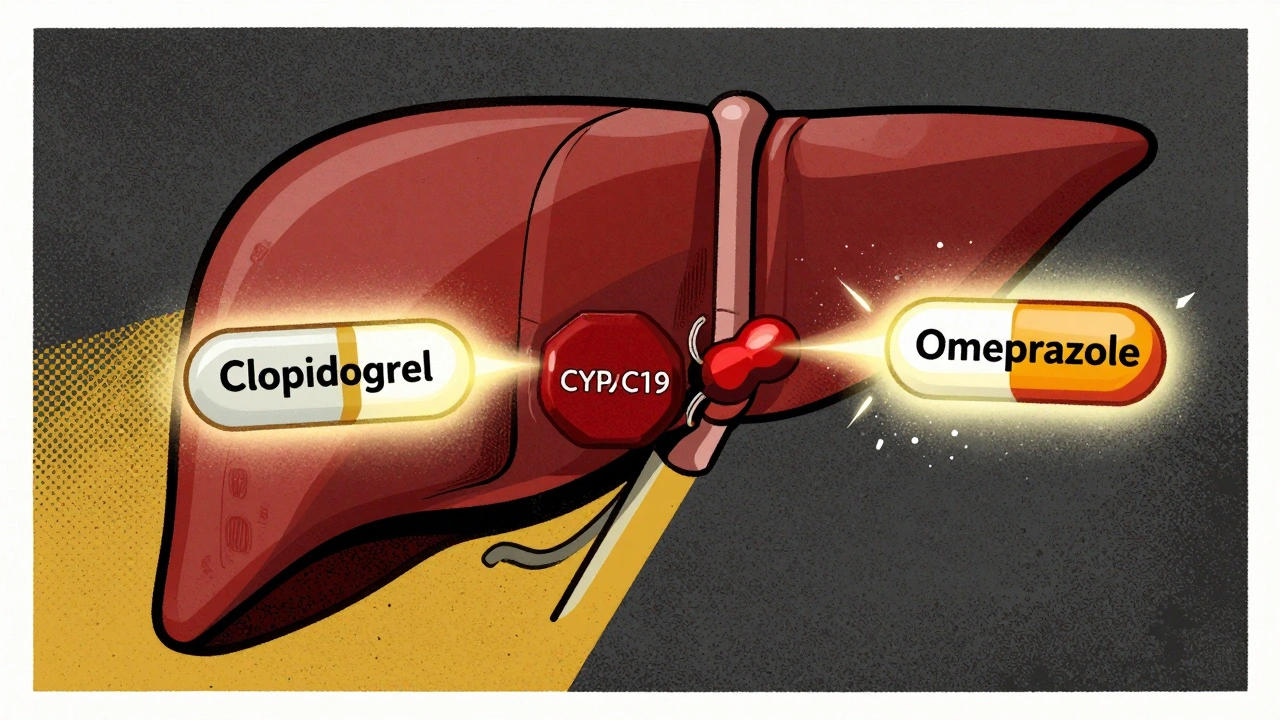
Clopidogrel isn’t active when you swallow it. It’s a prodrug - meaning your body has to turn it into something else to make it work. That something is an active metabolite that sticks to platelets and stops them from clumping. Without that metabolite, clopidogrel does nothing. And here’s the catch: your liver needs the enzyme CYP2C19 to make that metabolite. If CYP2C19 is blocked, clopidogrel can’t do its job.
This isn’t just a minor detail. About 30% of people in East Asia and 20-25% of Caucasians have a genetic variation that already reduces CYP2C19 activity. These are called intermediate or poor metabolizers. For them, clopidogrel is less effective even without any other drugs. Add omeprazole into the mix, and the problem gets worse.
Why Omeprazole Is the Problem
Omeprazole is a proton pump inhibitor (PPI). It’s great for heartburn, ulcers, and GERD. But it’s also one of the strongest inhibitors of CYP2C19 among all PPIs. Studies show that when you take 80 mg of omeprazole daily, it cuts the amount of clopidogrel’s active metabolite in your blood by up to 45%. Even the standard 20 mg dose reduces it by about 32%.
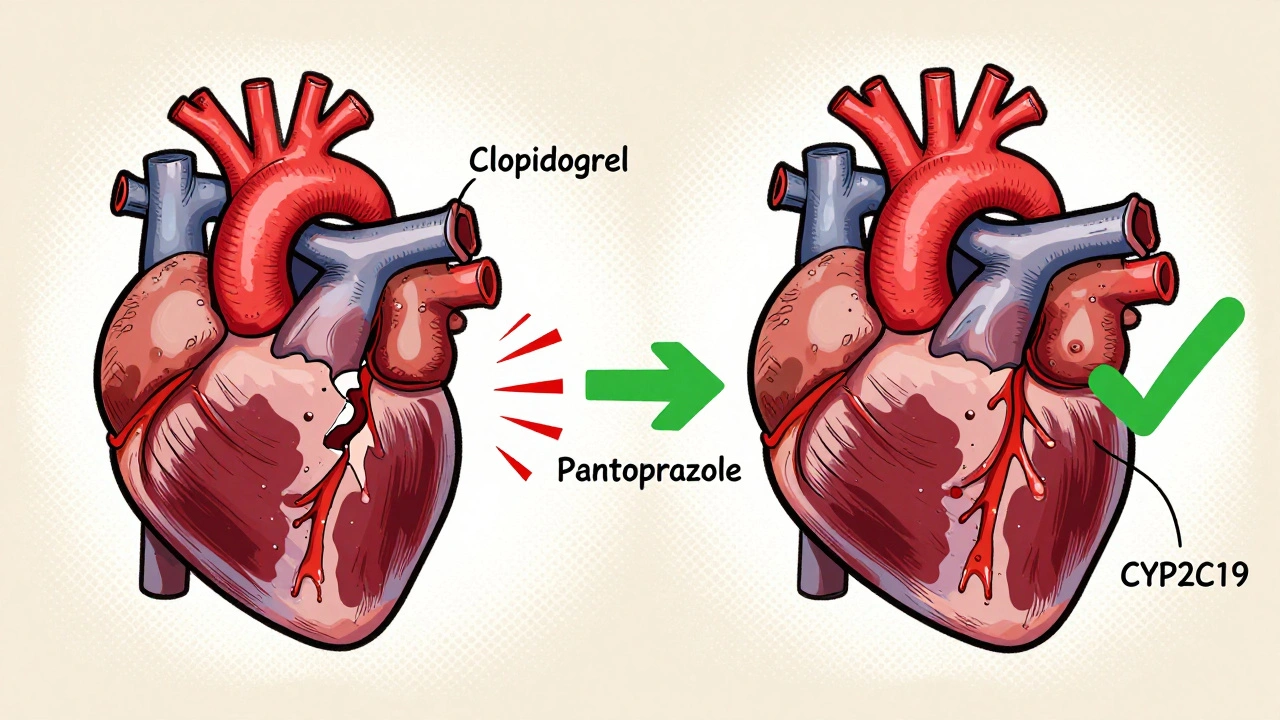
This isn’t guesswork. It’s measured in labs. The in vitro data shows omeprazole binds tightly to CYP2C19 with an IC₅₀ of just 2-4 μM - meaning it blocks the enzyme at very low concentrations. Compare that to pantoprazole (IC₅₀ 10-15 μM) or rabeprazole (15-20 μM). Omeprazole is the strongest. And because of that, the FDA issued a safety warning in 2009. The European Medicines Agency followed suit. Both say: avoid combining them.
Not All PPIs Are Created Equal
Here’s the good news: not every PPI interferes with clopidogrel the same way. If you need a stomach protector while on clopidogrel, you have better options.
- Omeprazole and esomeprazole (its isomer): Strong inhibition. Avoid.
- Lansoprazole: Mild effect at standard doses (30 mg). High doses (60 mg) may reduce clopidogrel’s effect by 18% - use cautiously.
- Pantoprazole: Minimal inhibition. Only about 14% reduction in clopidogrel exposure at 40 mg. Recommended as the safest PPI alternative.
- Rabeprazole: Slight reduction in peak levels (28%), but doesn’t affect overall exposure. A reasonable option if pantoprazole isn’t available.
- Ilaprazole: Newer PPI with almost no CYP2C19 inhibition. Still not widely available, but promising for the future.
Why does this matter? Because if you’re taking clopidogrel after a heart attack or stent placement, your life depends on it working. A 30-50% drop in active metabolite isn’t just a lab curiosity. It’s a real risk for clotting events.
The Clinical Evidence Is Mixed - But the Warning Stands
You might have heard that some big studies found no increased heart attacks or strokes when people took both drugs. The COGENT trial in 2010, with over 3,700 patients, showed no difference in cardiovascular events between those taking omeprazole and those who didn’t. The FAST-MI Registry in 2011 also found no link between PPI use and higher risk of death or heart attack.
But here’s what those studies didn’t tell you: they didn’t test everyone’s genes. They didn’t separate out poor metabolizers. And they didn’t measure clopidogrel’s active metabolite levels - they just counted events. That’s like saying a car engine runs fine because the dashboard light is green, even if the fuel line is clogged.
Meanwhile, a 2014 meta-analysis of over 270,000 patients found a 27% higher risk of cardiovascular events with PPI use - and omeprazole was the worst offender. In Asian populations, where CYP2C19 loss-of-function alleles are more common, the risk spikes even higher. One Korean study showed omeprazole cut clopidogrel’s effect by 54% in intermediate metabolizers.
So why the contradiction? Because clinical trials measure outcomes - not mechanisms. If a patient has a strong genetic profile and takes a low dose of omeprazole, they might be fine. But if they’re a poor metabolizer on a high dose? That’s where the danger lies. And we don’t always know who’s who.
What Should You Do?
If you’re on clopidogrel and need a PPI, here’s what the guidelines say:
- Avoid omeprazole and esomeprazole entirely. The FDA, ESC, and ACC all agree on this.
- Choose pantoprazole 40 mg daily. It’s the safest PPI option with the least interaction.
- Consider rabeprazole 20 mg daily if pantoprazole isn’t available.
- Don’t rely on timing. Taking clopidogrel in the morning and omeprazole at night doesn’t help. The inhibition happens in the liver, not the gut.
- Ask about H2 blockers. Famotidine is an alternative that doesn’t affect CYP2C19. It’s not as strong as PPIs for acid suppression, but it’s safe with clopidogrel.
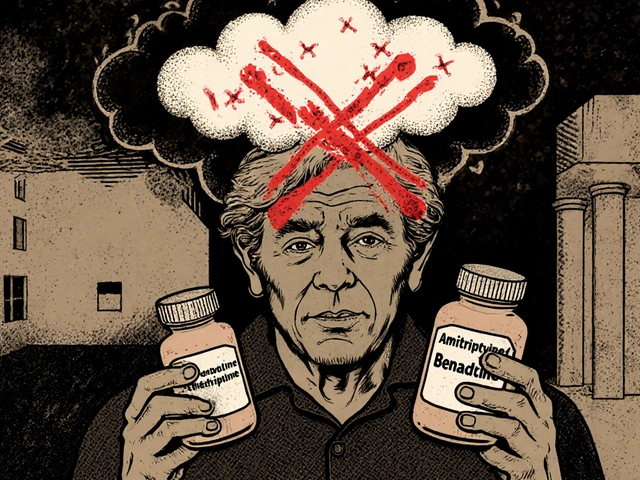
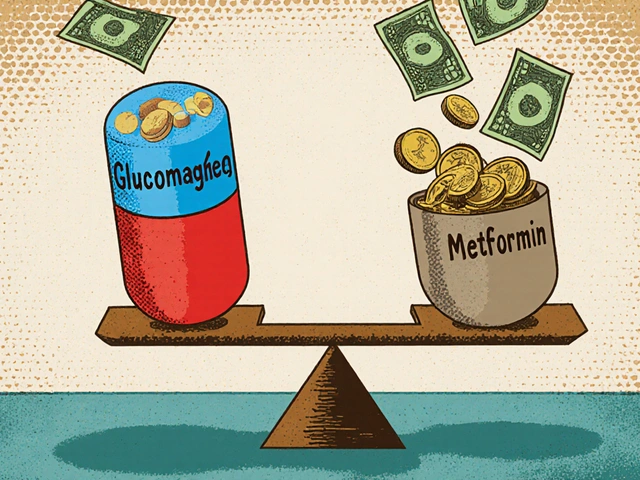
And if you’re at high risk - say, you had a stent placed last month - talk to your doctor about switching from clopidogrel to prasugrel or ticagrelor. These newer antiplatelets don’t rely on CYP2C19. They’re more expensive, but they’re not affected by PPIs. And for many patients, that’s worth it.
Genetic Testing Is Becoming Standard
Doctors used to guess who might be a poor metabolizer. Now, they can test. The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends CYP2C19 genotyping for anyone on clopidogrel who needs a PPI. If you’re a poor metabolizer (*2 or *3 allele), you should switch to prasugrel or ticagrelor - not just avoid omeprazole.
As of 2023, 74% of cardiology practices in the U.S. are doing some form of pharmacogenetic testing. It’s no longer experimental. It’s becoming routine. And it’s not just about omeprazole - it’s about making sure your medication works the way it’s supposed to.

What’s Changing in 2025?
The science keeps evolving. A 2025 study in Nature Scientific Reports confirmed that ilaprazole has the weakest CYP2C19 inhibition of any PPI tested. It barely touches clopidogrel’s metabolism. While it’s not yet widely available, it’s a sign of where things are headed.
The FDA’s 2023 draft guidance now uses a more precise model called the R-value to predict drug interactions. If R > 1.25, there’s clinical concern. Omeprazole scores above 1.5. Pantoprazole is below 1.1. That’s not a gray area anymore.
Three new antiplatelet drugs are in Phase II trials as of late 2024, designed to bypass CYP2C19 entirely. They’re not on the market yet, but they’re coming. And when they arrive, this whole debate might become obsolete.
Bottom Line
Don’t take omeprazole with clopidogrel. It’s not a maybe. It’s a clear, evidence-based warning. If you need stomach protection, pick pantoprazole or rabeprazole instead. If you’re at high risk for clots, ask about prasugrel or ticagrelor. And if you haven’t been tested for CYP2C19, ask your doctor - especially if you’re of Asian descent or had a recent stent.
This isn’t about fear. It’s about control. You’re taking clopidogrel to prevent a heart attack. Don’t let a common heartburn pill undo that. Make sure your meds work together - not against each other.
Can I take omeprazole and clopidogrel if I take them at different times of day?
No. Timing doesn’t help. The interaction happens in your liver, not your stomach. Whether you take omeprazole in the morning or at night, it still blocks the CYP2C19 enzyme long enough to reduce clopidogrel’s activation. Studies have tested separating doses by hours - and found no improvement in clopidogrel’s effectiveness.
Is pantoprazole really safer than omeprazole with clopidogrel?
Yes. Pantoprazole has the weakest effect on CYP2C19 among commonly used PPIs. At 40 mg daily, it reduces clopidogrel’s active metabolite by only about 14%, which is considered clinically insignificant. The American College of Gastroenterology and European Society of Cardiology both recommend pantoprazole as the preferred PPI for patients on clopidogrel.
What if I’m already taking omeprazole and clopidogrel together?
Don’t stop either drug on your own. Talk to your doctor. If you’re at low risk for heart events and have been on both for years without issues, your doctor might monitor you closely. But if you’ve had a stent, heart attack, or are a known CYP2C19 poor metabolizer, switching to pantoprazole or a different antiplatelet is strongly advised.
Are there natural alternatives to PPIs for heartburn?
There’s no proven natural substitute that matches PPIs for severe GERD or ulcers. H2 blockers like famotidine are a safer pharmaceutical option. Lifestyle changes - avoiding large meals, not lying down after eating, losing weight - can help reduce symptoms, but they don’t replace medication for high-risk patients.
Why do some doctors still prescribe omeprazole with clopidogrel?
Some doctors rely on older studies like COGENT or FAST-MI that didn’t show clear harm. Others may not be aware of the latest guidelines or genetic data. But major cardiology societies now clearly recommend avoiding omeprazole. If your doctor prescribes it, ask why - and whether they’ve considered your CYP2C19 status or alternatives like pantoprazole.
Does clopidogrel work differently in people of different ethnicities?
Yes. About 30-35% of East Asian populations carry CYP2C19 loss-of-function alleles (*2 or *3), compared to 20-25% in Caucasians. This means clopidogrel is naturally less effective in many Asian patients - and adding omeprazole makes it even worse. Studies in Korea and Taiwan show significantly greater loss of antiplatelet effect in these groups.
Next Steps
If you’re on clopidogrel and take any acid-reducing medication, check your prescription right now. Is it omeprazole or esomeprazole? If yes, schedule a call with your doctor or pharmacist. Ask: “Is there a safer alternative?” and “Should I get tested for CYP2C19?”
If you’re a caregiver or family member, help them track their meds. Write down every pill they take - including over-the-counter ones. Many people don’t realize omeprazole is in generic brands like Prilosec or store-label heartburn relief.
This interaction is preventable. You don’t need to choose between heart protection and stomach comfort. You just need the right information - and the right drugs.
Let’s be clear: this isn’t some theoretical pharmacology debate. This is life-or-death clinical reality. Omeprazole doesn’t just ‘interfere’ with clopidogrel-it actively sabotages it at the enzymatic level. The FDA didn’t issue that warning because someone got a funny feeling. It was because patients were having stent thromboses while taking both drugs, and the lab data showed metabolite levels plummeting. If you’re on clopidogrel post-stent and you’re still on omeprazole, you’re playing Russian roulette with your coronary arteries. The data is overwhelming. The guidelines are explicit. The only question is why anyone’s still prescribing this combo in 2025.
And don’t even get me started on the ‘timing doesn’t matter’ myth. I’ve seen residents try to justify taking them 12 hours apart like it’s some kind of clever hack. No. The enzyme inhibition is systemic, sustained, and irreversible for the drug’s half-life. The liver doesn’t care what time you took your pill. It just sees the inhibitor and shuts down CYP2C19. End of story.
Switch to pantoprazole. Or better yet, switch to ticagrelor. And if your doctor pushes back, ask them if they’ve read the 2024 CPIC update or if they’re still living in 2010. This isn’t opinion. It’s evidence-based medicine. Period.
Wow. Someone actually read the whole thing. 🙃
Meanwhile, my cousin’s cardiologist still prescribes omeprazole with clopidogrel like it’s 2008. He says ‘it’s fine’ and ‘I’ve never seen a problem.’ Guess what? Neither have I. But I also don’t have a PhD in pharmacokinetics. Maybe I should just stop taking my meds and drink apple cider vinegar instead? 🍎😂
There’s something deeply human about this interaction. We take drugs to extend life, to prevent suffering, to regain control. But we also take them because we’re afraid-afraid of pain, afraid of indigestion, afraid of being vulnerable. Omeprazole isn’t just a chemical; it’s a comfort. A shield against the discomfort of being alive. And clopidogrel? It’s a silent guardian, working in the dark, unaware that its power is being siphoned away by something meant to soothe.
So when we say ‘avoid omeprazole,’ we’re not just talking about enzymes. We’re asking people to trade one kind of fear for another. To accept that stomach discomfort might be better than a heart attack. That’s not just pharmacology. That’s philosophy. That’s the weight of choice in modern medicine.
And yet-we still don’t test enough. We still assume. We still guess. We treat bodies like machines, forgetting they’re shaped by genes, by ancestry, by history. The *2 allele isn’t a defect. It’s a variation. And maybe our failure to routinely test isn’t ignorance. Maybe it’s arrogance.
So… omeprazole = bad. Pantoprazole = good. Got it. Thanks for the 10-page essay on something I could’ve learned from a 3-sentence pharmacy handout. 🙄
Also, I typoed ‘pantoprazole’ as ‘pantoprazole’ in my notes. Hope you’re proud of me. 😘
This is such an important post-and so many people don’t know this! If you’re on clopidogrel, please, please check your meds. I had a friend who had a stent and was on omeprazole for years. She never felt different… until she had a mini-stroke. Turns out, her clopidogrel wasn’t working. Switched to pantoprazole, got tested for CYP2C19, and now she’s doing great. You don’t need to be scared-just informed. Talk to your pharmacist. They’re the real heroes here. 💪❤️
Okay but why does this feel like a betrayal? I’ve been taking Prilosec for 8 years. It’s my little daily ritual. Now you’re telling me it’s secretly sabotaging my heart meds?? I’m not mad… I’m just disappointed. 😔
Also, can we talk about how weird it is that the drug companies know this but still sell omeprazole like it’s harmless? Like… who’s making money off this? 😅
While the empirical data presented in this post is statistically significant and methodologically sound, one must interrogate the epistemological foundations of the clinical recommendations. The COGENT trial, while underpowered for pharmacogenomic stratification, remains a randomized controlled trial-the gold standard of evidence. To privilege in vitro IC50 values and post hoc meta-analyses over prospective outcomes is to commit the ecological fallacy. Furthermore, the assertion that pantoprazole is ‘clinically insignificant’ in its interaction is itself an oversimplification of pharmacokinetic variability across populations. One cannot ignore interindividual metabolic variance, nor the confounding influence of concomitant CYP3A4 inducers. Until we account for these factors in prospective, genotype-stratified trials, we risk replacing one dogma with another.
Moreover, the implicit assumption that genetic testing is ‘routine’ in 74% of U.S. cardiology practices is misleading. The actual rate of *actionable* testing-where results lead to therapeutic change-is closer to 18%. The rest are performative compliance. We are not advancing medicine. We are performing it.
Just switched from omeprazole to pantoprazole after reading this. My heart feels lighter. Seriously. Thanks for the clarity. 💙
Man, this whole thing is wild. It’s like your body’s got a secret club of enzymes, and omeprazole is the guy who shows up with a crowbar and says, ‘Nah, we’re not doing that today.’ 🤯
And the kicker? The liver doesn’t even care if you’re ‘just taking it at night.’ It’s like trying to whisper a secret to someone while your neighbor is blasting metal through a wall. Doesn’t matter when you whisper-it’s still drowned out.
Also, I just Googled ‘ilaprazole’ and found out it’s basically the superhero PPI no one’s heard of yet. I’m gonna start calling it ‘Clopidogrel’s Best Friend.’ 🦸♂️💊
Big shoutout to the pharmacists who actually know this stuff. We need more of you. And less of the docs who still think ‘timing’ fixes everything. 😅