Every year, over a million people in the U.S. end up in the emergency room because of unexpected reactions between their medications. Many of these cases aren’t accidents-they’re preventable. The biggest missing piece? Asking the right questions before you take that new pill, supplement, or even that grapefruit juice with your breakfast.
Why Drug Interactions Happen
Drug interactions aren’t rare. They happen when one substance changes how another works in your body. This could mean a medication becomes less effective, causes stronger side effects, or even triggers a dangerous reaction. There are three main types:- Drug-drug interactions: When two or more medications react. For example, taking blood thinners like warfarin with certain antibiotics can increase your risk of bleeding.
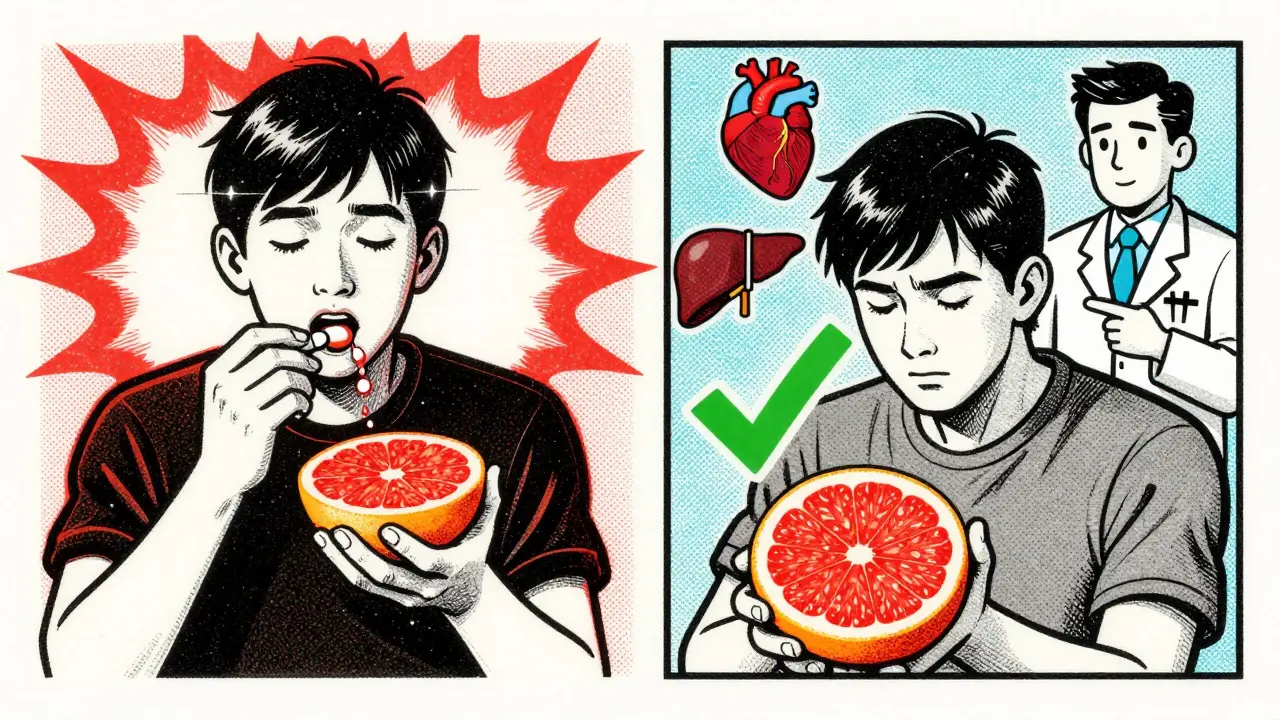
- Drug-food/beverage interactions: Grapefruit juice can block how your body breaks down some cholesterol and blood pressure meds, leading to dangerous buildup. Alcohol can make sedatives or painkillers more potent-and more risky.
- Drug-condition interactions: If you have high blood pressure, decongestants in cold medicines can spike your pressure to unsafe levels. If you have kidney disease, some pain relievers like ibuprofen can make things worse.
The FDA requires all prescription labels to warn about known interactions, but those warnings don’t always cover everything-especially if you’re taking supplements, herbal products, or over-the-counter meds. That’s why you need to talk to your pharmacist.
What to Ask Your Pharmacist
Pharmacists are trained to spot hidden risks. But they can’t help if you don’t tell them everything. Here are the exact questions to ask when you pick up a new prescription or add something to your routine:- Can this medicine interact with anything else I’m taking? Don’t just list your prescriptions. Include every supplement, vitamin, herb, or over-the-counter drug-even if you think it’s harmless. St. John’s wort, for example, can make birth control, antidepressants, and heart meds stop working properly.
- Should I avoid any foods, drinks, or alcohol? Grapefruit juice affects more than 85 medications, including some statins, blood pressure drugs, and anti-anxiety pills. Aged cheeses, cured meats, and red wine can be dangerous if you’re on MAO inhibitors like phenelzine. Even a single glass of wine can cause a spike in blood pressure with these drugs.
- Will this affect my existing health conditions? If you have diabetes, heart disease, liver problems, or kidney issues, some medications can make them worse. Ask specifically: “Is this safe for someone with my condition?”
- When and how should I take this? Some drugs need to be taken on an empty stomach. Others must be taken with food to reduce nausea or improve absorption. Taking them at the wrong time can change how they interact with other meds. For example, thyroid medication should be taken alone, at least 30-60 minutes before eating or taking other pills.
- What side effects should I watch out for? Not all side effects are obvious. Signs of a bad interaction include sudden dizziness, unusual bruising or bleeding, chest pain, confusion, rapid heartbeat, or swelling. Know what’s normal and what’s not.
- Do I need to adjust my dose if I start or stop another medication? Sometimes, adding a new drug means you need to lower the dose of an old one. This is common with antidepressants, seizure meds, and blood thinners.
- Are there any alternatives if this one has too many risks? If your new prescription has a long list of warnings, ask if there’s another option with fewer interactions. Pharmacists often know of equally effective alternatives that are safer for your current regimen.
What to Bring to Your Appointment
Don’t rely on memory. Bring a written list of everything you take, including:- Prescription names and dosages
- How often you take each one
- Over-the-counter pills (like ibuprofen, antacids, or sleep aids)
- Vitamins and minerals (especially iron, calcium, vitamin K, or vitamin D)
- Herbs and supplements (turmeric, fish oil, ginkgo, echinacea, etc.)
- Any recreational substances (including alcohol and cannabis)
Also note your diet habits. Do you drink grapefruit juice daily? Do you eat a lot of leafy greens? Do you have a glass of wine with dinner? These details matter.
Why Pharmacists Are Your Best Line of Defense
Pharmacists don’t just fill prescriptions-they review your whole picture. In 2023, a study in the Journal of the American Pharmacists Association found that when pharmacists did full medication reviews with Medicare patients, drug interaction incidents dropped by nearly 24%. That’s not a small number. It’s life-saving.Many pharmacies now use digital tools that flag interactions automatically. But those systems only work if your profile is complete. If you switch pharmacies or forget to update your list, the system misses things. That’s why your verbal conversation with your pharmacist is still essential.
Special Cases to Watch Out For
Some medications are especially tricky:- Warfarin (Coumadin): Interacts with vitamin K (found in spinach, kale, broccoli), cranberry juice, and many antibiotics. Even small changes in your diet can throw off your INR levels.
- Statins (like atorvastatin): Grapefruit juice can cause muscle damage. Avoid it entirely if you’re on these.
- SSRIs (like sertraline): Can interact dangerously with St. John’s wort, leading to serotonin syndrome-a rare but life-threatening condition.
- Diabetes meds: Some antibiotics and steroids can spike your blood sugar. Others can cause hypoglycemia when mixed with alcohol.
- Heart rhythm drugs (like amiodarone): Can be affected by grapefruit, certain antibiotics, and even some antacids.
And don’t forget: supplements aren’t regulated like drugs. A “natural” product can still be powerful-and dangerous. Turmeric can thin your blood. Calcium can block absorption of thyroid meds. Iron can interfere with antibiotics. Always ask.

When to Talk to Your Pharmacist
Don’t wait for a problem to happen. Talk to your pharmacist:- Every time you get a new prescription
- When you start or stop a supplement
- After a hospital visit or doctor’s appointment
- Every 3-6 months, even if nothing changed
Why? The most common cause of a bad interaction? The newest medication added. It’s not always the old ones-it’s the one you just started.
Final Tip: Keep It Simple, Keep It Updated
Write down your meds on a card or in your phone. Keep it updated. Show it to every pharmacist, every doctor, every ER nurse. You wouldn’t drive without checking your fuel gauge. Don’t take meds without checking your interaction gauge.Medication safety isn’t just about following instructions. It’s about asking questions, sharing details, and staying involved. Your pharmacist is your partner-not just a dispenser. Use them.
Can I just check for drug interactions online instead of asking my pharmacist?
Online tools can help, but they’re not enough. Most don’t know your full medical history, diet, or supplement use. They also don’t account for how your body processes drugs based on age, liver function, or kidney health. Pharmacists use clinical judgment, not just algorithms. A website might miss that your grapefruit juice habit combined with your new statin could cause muscle damage. Your pharmacist won’t.
Do I need to tell my pharmacist about vitamins and herbs?
Yes. Absolutely. Many people think vitamins are harmless, but they’re not. Vitamin K can reduce the effect of warfarin. Fish oil and garlic supplements can increase bleeding risk when taken with blood thinners. St. John’s wort can make birth control, antidepressants, and heart meds stop working. Pharmacists need the full picture to keep you safe.
What if I forget to mention something I’m taking?
It happens. But the sooner you update your list, the better. Call your pharmacy if you realize you forgot to mention a supplement, new OTC drug, or even a change in your alcohol intake. Many pharmacies offer free medication reviews-you can schedule one anytime. Don’t wait for a side effect to show up.
Can my pharmacist change my prescription if there’s a risk?
No, only your doctor can change your prescription. But your pharmacist can strongly recommend an alternative and contact your doctor on your behalf. Many pharmacists have collaborative practice agreements that let them suggest safer options. If your current drug has too many interaction risks, ask your pharmacist to help you find a better one.
Are drug interactions more dangerous for older adults?
Yes. People over 65 are more likely to take five or more medications daily. Their bodies process drugs slower, and they’re more sensitive to side effects. According to CDC data, seniors account for nearly half of all drug interaction-related ER visits. That’s why medication reviews are especially critical for older adults.




I've been a pharmacist for 18 years and I still get surprised by what people don't tell me. Like the guy who took turmeric for 'inflammation' and ended up in the ER with a bleeding ulcer. He didn't think it counted as a 'medication.' It's not just about the big stuff-it's the little things you think are harmless.
The pharmacokinetic interplay between CYP450 substrates and inhibitors is profoundly underappreciated by the lay public-particularly with regard to grapefruit furanocoumarins inhibiting CYP3A4-mediated first-pass metabolism, thereby elevating serum concentrations of statins, calcium channel blockers, and even some benzodiazepines. The clinical implications are non-trivial, and often under-documented in consumer-facing resources.
they dont want you to know this but pharmacies are owned by big pharma and they want you to keep taking meds... why else would they not tell you about the natural cures? i heard a guy cured his high blood pressure with garlic and apple cider vinegar and now he's suing the hospital for not telling him
The systematic integration of pharmacist-led medication reconciliation protocols has demonstrated statistically significant reductions in adverse drug events across longitudinal cohort studies. It is incumbent upon healthcare systems to institutionalize these practices as standard of care, particularly within geriatric populations where polypharmacy prevalence exceeds 80%.
I find it rather amusing that this article treats pharmacists as some kind of infallible oracle. They're not doctors. They're not even nurses. They're glorified cashiers with a pharmacy degree who read off a computer screen and sometimes forget to ask if you're allergic to penicillin. I've had more accurate advice from a Reddit thread.
the fda knows about all these interactions but they let them slide because they make more money off you being sick... and don't get me started on how they suppress natural remedies. you think grapefruit juice is bad? try avoiding the glyphosate in your kale and the aluminum in your antacids. they're all connected.
Warfarin + vitamin K = unstable INR. Statins + grapefruit = rhabdo risk. SSRIs + St. John’s wort = serotonin syndrome. These aren’t rumors. They’re in the Lexicomp database. If you’re on more than three meds, get a med review. It’s free. Do it.
This is so important. My uncle had a bad reaction because he took ibuprofen with his blood thinner and didn’t think it mattered. He’s fine now, but it scared us all. I now keep a printed list and show it to every new provider. Simple, but it saves lives.
America is falling apart because people won't take responsibility for their own health. You think a pharmacist is going to babysit you? Get your act together. Read the damn label. If you can't, don't take it.
It is not merely a matter of pharmacological interaction, but rather a systemic failure of patient education, compounded by the commodification of healthcare delivery. The pharmaceutical-industrial complex incentivizes polypharmacy, while simultaneously disempowering the patient through obfuscation, jargon, and institutionalized apathy. One cannot reasonably expect a layperson to navigate a labyrinth of CYP450 isoforms, P-glycoprotein transporters, and bioavailability modifiers without professional guidance-yet, we have allowed this burden to be placed upon the individual. This is not negligence; it is structural malfeasance.
they only tell you about the big ones. what about the 500 other meds they don't list? i read a study that said 92% of drug interactions are hidden because the FDA only tests them in isolation. your pharmacist? they're just reading a database that's 10 years old. you're a lab rat.
I used to think supplements were safe. Then my mom had a stroke after mixing fish oil with her blood thinner. She’s fine now, but I learned the hard way. I bring a list to every appointment. No excuses. If you’re taking anything, say it. Even if it’s ‘just’ melatonin.