Every year, hundreds of thousands of people end up in the hospital not because their condition got worse, but because two perfectly safe medications were taken at the wrong time. You might be on blood thinners, thyroid pills, antibiotics, or supplements-and if you’re taking them all at once with your morning coffee, you could be reducing their effectiveness-or even putting yourself at risk. The solution isn’t always to stop one of your meds. Sometimes, it’s as simple as waiting a few hours between doses.
Why Timing Matters More Than You Think
Not all drug interactions are the same. Some happen because two drugs compete for the same enzyme in your liver. Others happen because one drug binds to another in your stomach like glue. The first kind? Timing won’t help. The second kind? Timing can save your treatment. Take antibiotics like ciprofloxacin. If you take it with an antacid like Tums or Maalox, the aluminum or magnesium in the antacid grabs onto the antibiotic and stops your body from absorbing it. Studies show absorption drops by up to 90%. That means your infection doesn’t get treated. But if you wait just two hours after the antacid before taking the antibiotic? You get nearly full absorption. Same dose. Same effectiveness. Just better timing. Same goes for levothyroxine, the common thyroid medication. If you take it with iron, calcium, or even a multivitamin, your body absorbs less than half of what it should. A 2019 study in the Journal of Clinical Endocrinology & Metabolism found that spacing levothyroxine four hours apart from these supplements keeps absorption at 95%. That’s the difference between feeling tired all day and having your energy back.Which Medications Need Special Timing?
Some drug pairs are notorious for timing issues. Here are the most common ones-and exactly how long to wait:- Antibiotics (tetracycline, doxycycline) + Dairy or Calcium: Wait 2-3 hours. Milk, yogurt, and calcium supplements bind to these antibiotics and block absorption.
- Levothyroxine + Iron, Calcium, or Aluminum-containing products: Wait 4 hours. This includes antacids, multivitamins, and even some fiber supplements.
- Bisphosphonates (alendronate, risedronate) + Food or other meds: Take on an empty stomach with plain water, then wait at least 30 minutes before eating or taking anything else.
- Fluoroquinolones (ciprofloxacin, levofloxacin) + Antacids, iron, or zinc: Separate by 2 hours.
- Proton pump inhibitors (PPIs) + Iron supplements: PPIs reduce stomach acid, which your body needs to absorb iron. Wait at least 2 hours after the PPI before taking iron.
- Clarithromycin + Colchicine: This combo can cause deadly muscle toxicity. Separate by at least 2 hours, or better yet, ask your doctor if you can avoid the combination entirely.
These aren’t guesses. These are numbers from the FDA’s 2021 labeling guidelines and peer-reviewed studies. The key is knowing which ones apply to you.
What Timing Won’t Fix
Not every interaction can be solved by waiting. If two drugs affect the same liver enzyme-like warfarin and metronidazole-timing won’t help. Metronidazole shuts down the enzyme that breaks down warfarin, so warfarin builds up in your blood. That increases bleeding risk, no matter when you take them. Same with statins and grapefruit juice. Grapefruit blocks an enzyme in your gut that normally breaks down statins. That means more drug enters your bloodstream. You can’t time your way out of that. You either stop the grapefruit or switch statins. These are metabolic interactions. They need dose changes, drug swaps, or complete avoidance-not scheduling tricks. Timing only works for absorption-based problems-when one drug physically blocks another from being absorbed in your gut.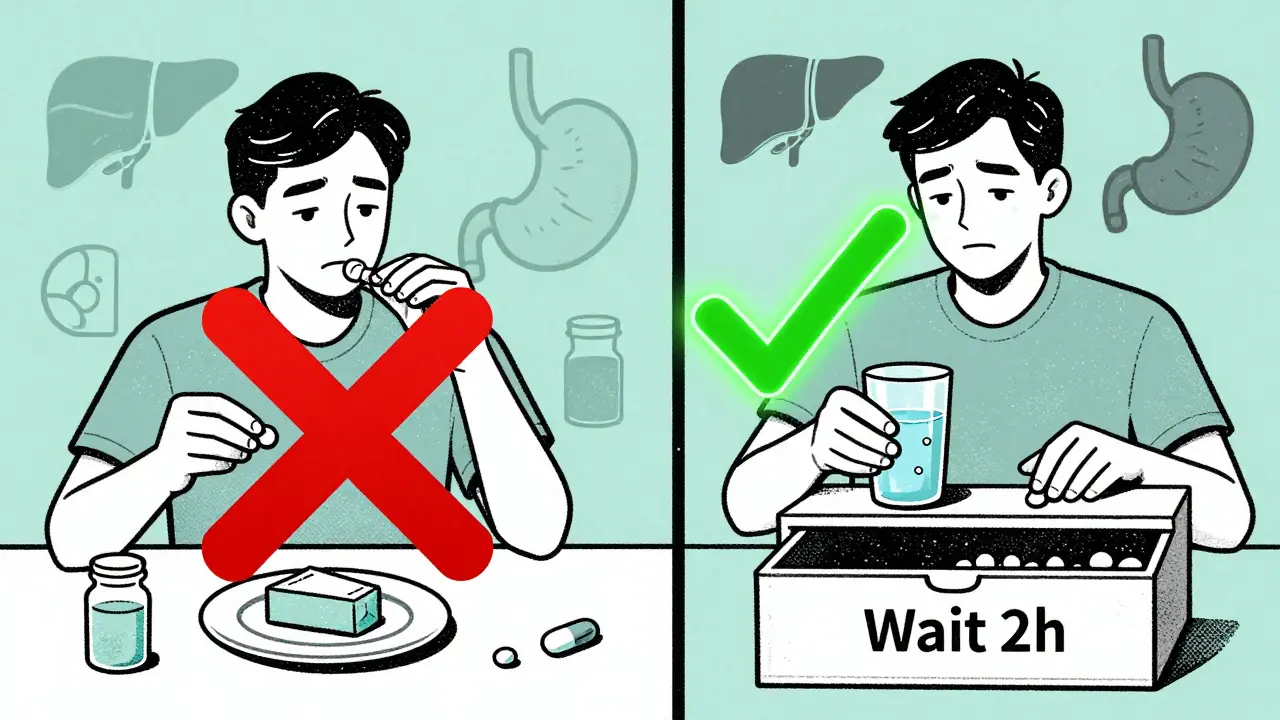
Why Hospitals Are Getting Better at This
Hospitals have been using computer systems since the mid-2000s to catch these timing issues. The Dutch national drug database, the G-standard, started flagging time-dependent interactions back in 2006. Today, 82% of U.S. hospitals have similar systems built into their electronic records. These systems don’t just say “possible interaction.” They say: “Ciprofloxacin and calcium may reduce absorption. Separate by 2 hours.” They even suggest exact times: “Take ciprofloxacin at 8 a.m., calcium at 10 a.m.” But here’s the catch: these systems still trigger false alarms about 45% of the time. Why? Because they don’t know your actual schedule. If you take your calcium at 6 p.m. and your antibiotic at 8 p.m., the system still flags it-even though you’re fine. That’s why doctors and pharmacists still need to double-check.What Happens When Timing Isn’t Followed
The Dutch Medicines Evaluation Board found that 18% of preventable adverse drug events in Europe come from people not following timing instructions. In the U.S., the FDA estimates that 20-30% of all drug interactions could be avoided just by spacing doses. One real case: a 72-year-old woman on levothyroxine and iron pills. She took them together every morning. Her TSH levels stayed high. Her doctor kept increasing her thyroid dose-thinking she wasn’t absorbing enough. But she was. The iron was blocking it. Once she switched to taking iron at night, her thyroid levels normalized in six weeks. No dose change. Just better timing. Another example: a man on ciprofloxacin for a UTI took his calcium supplement with breakfast. His infection didn’t clear. He went back to the doctor. They asked about timing. He hadn’t been told to wait. He waited two hours. Infection gone in three days.How to Get Your Timing Right
If you take five or more medications, you’re at high risk. Here’s how to fix it:- Make a full list of everything you take. Include prescriptions, over-the-counter drugs, vitamins, herbs, and supplements. Don’t forget antacids or fiber pills.
- Check for known timing issues. Use trusted sources like Lexicomp, Micromedex, or the FDA’s drug interaction database. Ask your pharmacist-they’re trained for this.
- Map out your day. Write down when you take each med. Group them by timing needs. For example: “Take thyroid on empty stomach. Wait 4 hours before iron or calcium.”
- Use tools to help. Pill organizers with morning/afternoon/evening compartments reduce errors by 43%. Apps like Medisafe let you set custom alerts for each dose and spacing window. A 2021 trial showed a 57% improvement in adherence with these tools.
- Ask your doctor or pharmacist: “Is there a timing issue with any of my meds?” Don’t assume they know. Many providers still don’t think about it.
Common Mistakes and How to Avoid Them
Most people fail at timing because they overcomplicate it-or ignore it entirely.- Mistake: Taking all your pills at once because it’s easier.
- Solution: Use a color-coded chart. Red for “must wait 4 hours,” green for “can take with food.”
- Mistake: Skipping a dose because you forgot the timing rule.
- Solution: Set two phone alarms-one for the first med, one for the second, with a 2- or 4-hour gap.
- Mistake: Assuming your doctor already knows.
- Solution: Bring your list to every appointment. Say: “I’m worried about interactions. Can we check the timing?”
One nurse in California tracked 120 elderly patients over 18 months. Those who used a simple printed schedule with clear timing instructions had 32% fewer cases of iron deficiency anemia. The others? Their levels kept dropping.
What’s Next for Medication Timing
The future is personal. New systems like Epic’s 2023 update now consider your kidney function, stomach pH, and even your genetic profile to suggest timing. If you’re a slow metabolizer of certain drugs, the system might recommend longer gaps. The FDA is pushing for more labeling that includes timing advice. By 2028, experts estimate that better timing protocols could prevent 115,000 to 178,000 hospital visits in the U.S. each year-and save $1.2 to $1.8 billion. But none of that matters if you don’t know your own schedule. The technology is here. The data is clear. The solution is simple: space your meds.Can I just take my medications at night instead of morning to avoid interactions?
Sometimes, yes-but only if it doesn’t interfere with the drug’s purpose. For example, levothyroxine must be taken on an empty stomach, first thing in the morning, because food blocks absorption. Taking it at night might work if you haven’t eaten for 4+ hours. But for blood pressure meds or diuretics, nighttime dosing might cause you to wake up to use the bathroom. Always check with your doctor before changing timing.
What if I forget to wait the full 2 or 4 hours?
If you accidentally take them together, don’t panic. One mistake won’t ruin your treatment. But don’t make it a habit. If it happens often, talk to your pharmacist. They can suggest alternatives, like switching to a different antibiotic or a different form of calcium that doesn’t interfere. For critical meds like levothyroxine, repeated mistakes can lead to under-treatment and long-term health problems.
Do I need to space out all my medications?
No. Only specific combinations have timing issues. Most medications can be taken together safely. The key is identifying which ones need separation. A pharmacist can review your list and tell you exactly which pairs require spacing. Don’t assume everything needs a gap-most don’t.
Are natural supplements safe to take with my prescriptions?
Many aren’t. Calcium, iron, magnesium, and even fiber supplements can block absorption of antibiotics, thyroid meds, and bone drugs. Herbal supplements like St. John’s Wort can interfere with metabolism of antidepressants and birth control. Always treat supplements like drugs-they can interact, sometimes dangerously. Always tell your doctor what you’re taking.
Why don’t my doctors always mention timing?
Many doctors aren’t trained to think about timing as a tool. They focus on which drugs to prescribe, not when to take them. Pharmacists are better trained for this. If your doctor doesn’t mention it, ask. Say: “I’ve heard timing matters for some meds. Can you check if any of mine need spacing?” Most will appreciate the question-and look it up.




I used to take my levothyroxine with my morning multivitamin-until I started feeling like a zombie at 11 a.m. My pharmacist caught it during a routine check. Four-hour gap? Game changer. I now take my thyroid first thing, coffee after, and supplements at dinner. Energy’s back, and my TSH is perfect. Simple fix, huge difference.
Don’t overthink it. Just write it down. I keep a sticky note on my fridge.
Let me get this straight-you’re telling me the entire medical establishment has been asleep at the wheel for decades because nobody thought to ask, ‘What if you just… wait?’
What’s next? ‘Hey, maybe drinking water before your pills helps?’
This isn’t science. It’s common sense that got buried under a mountain of pharmaceutical bureaucracy. We’re being sold a miracle cure: time.
And it’s free.
How dare they.
Timing isn’t just about chemistry-it’s about rhythm. Our bodies aren’t machines with on-off switches; they’re symphonies of enzymes, acids, and circadian whispers. When you jam a calcium tablet into your gut like a brick in a clock, you don’t just block absorption-you disrupt the whole melody.
Levothyroxine at dawn? That’s not a pill-it’s a ritual. A quiet bow to your thyroid’s natural pulse. And ciprofloxacin after a Tums? That’s not a mistake-it’s a betrayal of biochemistry.
People think medicine is about pills. It’s not. It’s about harmony. And harmony requires patience.
So wait.
Wait for the gut to settle.
Wait for the stomach to forget.
Wait for your body to remember how to heal.
Why are Americans so lazy? You take your pills at the same time because you’re too busy scrolling TikTok. In India, we’ve been doing this for generations-take medicine with water, not with food, not with tea, not with milk. No apps. No alarms. Just discipline.
My grandmother took her blood pressure meds at 5 a.m. sharp, no exceptions. No one told her about FDA guidelines. She just knew.
You don’t need technology. You need respect.
OMG I JUST REALIZED I’VE BEEN TAKING MY IRON WITH MY THYROID FOR 3 YEARS 😭
Thank you thank you thank you for this post. I’m going to rewrite my whole schedule tonight. I even bought one of those pill boxes with AM/PM slots-now I’m gonna label each one with colors like you said. Red for wait 4 hours, green for chill. I’m so excited I might cry. This is life-changing stuff.
Also-can we start a subreddit for medication timing? I’ll be the admin. I have spreadsheets.
Absorption-based interactions: timing works.
Metabolic: timing doesn’t.
Pharmacokinetics > pharmacodynamics.
Check Lexicomp. Consult pharmacist.
Don’t guess.
So… I’ve been taking my cipro with my calcium gummies since last Tuesday. I’m gonna die, right?
Just kidding. Kinda.
But seriously-this is the most useful thing I’ve read all year. I used to think ‘drug interactions’ meant ‘you’ll explode.’ Turns out it’s more like ‘you’re just wasting your money and feeling tired.’
Also, why does no one ever tell you this? I feel like I’ve been gaslit by the medical system.
This is so important. I’ve seen elderly patients get confused, overwhelmed, and give up-because they’re told to take 8 pills a day and nobody explains how to space them. One woman took her antibiotics with her oatmeal because ‘it’s easier.’ Her UTI never cleared.
We need more of this. Not just for patients, but for caregivers. A simple chart, printed and taped to the fridge, can save someone from hospitalization.
Pharmacists are the real heroes here. If you have one you trust, hug them.
I used to think I was ‘too busy’ to care about timing. Then my mom had a stroke from a warfarin interaction with an herbal supplement she didn’t even think was a drug. She’s fine now-but we’re not taking any chances.
I made a color-coded chart for her. Green for safe. Red for ‘wait 4 hours.’ Yellow for ‘ask the pharmacist.’
She doesn’t read much, but she reads colors. Now she takes everything right. No more confusion. No more panic.
This isn’t just medicine. It’s love in action.
Another overhyped article. Everyone knows you don’t take antibiotics with milk. This is basic. Why is this even a post?
Also, 82% of U.S. hospitals use systems? Cool. But 45% false alarms? That’s just noise. And noise doesn’t save lives.
Just take your meds. Stop overcomplicating.
i took my iron and thyroxine together for years... i never knew it was a problem. my doctor never said anything. now i feel so dumb. but thank you for posting this. i changed my schedule tonight. hope it helps.
Think about it: time is the only thing we can’t buy, can’t steal, can’t hack. And yet, in the age of AI and quantum computing, the most powerful tool we have for safe medication use is… waiting. Not a pill. Not a device. Not a gene edit. Just… pause. Breathe. Let your gut rest. Let chemistry do its quiet work.
Our civilization has mastered the atom, mapped the genome, and sent probes to Pluto-but we still can’t get people to wait two hours between a pill and a yogurt.
That’s not a medical failure.
That’s a spiritual one.
We’ve forgotten patience.
We’ve forgotten reverence for the body’s slow, silent wisdom.
Maybe the real interaction isn’t between drugs.
It’s between us and time.
Just read your comment, Manish. That’s beautiful. I didn’t think about it like that. I’ve been treating my meds like chores. But you’re right-it’s a kind of respect. Like tending a garden. You don’t dump fertilizer on a seedling right after planting. You wait. You listen. You let it grow.
Thanks for that.