When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. But what happens when that pill starts breaking down before its expiration date? Stability isn’t just a technical term-it’s the difference between a safe, effective medicine and one that could harm you. Many people assume expiration dates are arbitrary, but they’re based on years of scientific testing to ensure the drug stays potent, safe, and physically intact. For generic drugs, however, this process isn’t always straightforward.
What Stability Testing Actually Measures
Stability testing isn’t about checking if a pill looks right on the shelf. It’s a rigorous, multi-part analysis that tracks how a drug changes over time under real-world conditions. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require four key areas to be monitored: chemical, physical, microbiological, and functional stability.Chemical stability looks at whether the active ingredient breaks down into harmful byproducts. High-Performance Liquid Chromatography (HPLC) is the standard tool here, catching impurities as small as 0.1% of the original dose. Even tiny amounts can be dangerous-some degradation products are toxic, while others simply make the drug useless.
Physical stability checks appearance, texture, and how well the drug dissolves in your body. A tablet might look fine, but if it doesn’t break down properly in your stomach, you won’t absorb the medicine. For liquid formulations, viscosity matters. If it thickens too much, an inhaler won’t spray correctly. For nanoparticles used in advanced treatments, like those for cystic fibrosis, particles must stay under 200 nanometers. If they clump together, they lose their ability to reach targeted cells.
Microbiological stability ensures no mold, bacteria, or yeast grows in the product. Non-sterile drugs can’t have more than 100 colony-forming units per gram. Sterile injectables must meet an even stricter standard: a 1 in 1 million chance of contamination. Preservatives can fail if the product’s pH or water activity shifts-even slightly-during storage.
Functional stability applies to delivery systems. An inhaler must deliver the exact same dose every time. A metered-dose inhaler must release between 90% and 110% of its labeled dose. If it doesn’t, patients with asthma or COPD could be at risk.
How Shelf Life Is Determined-and Why It’s Often Wrong
Most companies use two types of testing: real-time and accelerated. Real-time means storing the drug at normal room temperature (24-25°C) and checking it every few months for up to three years. Accelerated testing crams years of aging into months by using higher heat (40°C) and humidity (75%).Here’s the problem: accelerated testing doesn’t always predict real-world failure. In one case, a company ran accelerated tests on a generic thyroid medication and saw no degradation. But after 24 months in real storage, the tablets crystallized. The drug was still chemically intact-but physically useless. The company lost $250,000 and 18 months of work.
Why? Because some degradation pathways only happen at lower temperatures over long periods. A chemical reaction that takes years to form at room temperature might not show up at 40°C because a different reaction dominates. This is why experts warn against blindly trusting accelerated data.
And then there’s storage documentation. The FDA issues Form 483 warnings for this all the time. Saying a product is stored at “room temperature” isn’t enough. You must record actual temperature logs. If the warehouse hits 32°C for a week during summer, that’s a red flag-even if the expiration date says 24 months.
Why Generic Drugs Are More Vulnerable
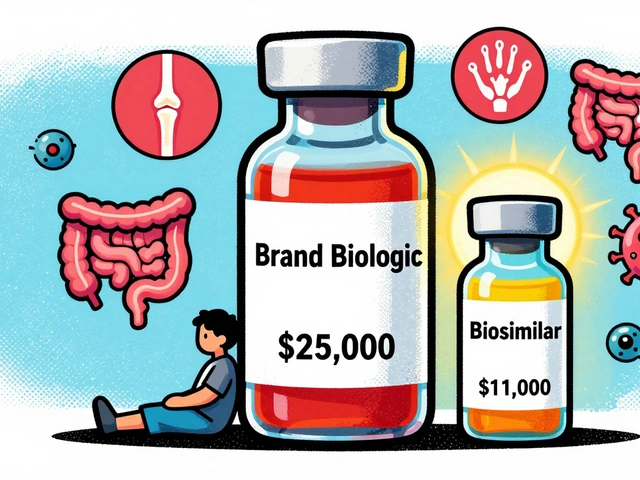
Generic drugs are cheaper because they don’t repeat the expensive clinical trials of brand-name drugs. But they do need to prove they’re bioequivalent-meaning they deliver the same amount of active ingredient into the bloodstream.What they don’t always prove is that they’re equally stable. Differences in excipients-fillers, binders, coatings-can drastically change how a drug behaves over time. A 2020 FDA study found that 17.3% of generic levothyroxine products had stability issues that the brand-name version (Synthroid) didn’t. Why? Moisture. One generic used a less effective coating, allowing humidity to seep in and destabilize the active ingredient.
Even small changes in manufacturing can have big effects. A change in the drying process of a tablet can alter its porosity. That might seem minor, but it affects how quickly moisture gets in. And once moisture gets in, degradation accelerates.
For patients on long-term medications-like blood thinners, antidepressants, or thyroid drugs-this isn’t just a technical issue. A 10% drop in potency can mean a seizure, a clot, or a relapse.
Real-World Consequences of Poor Stability
In 2022, the Parenteral Drug Association surveyed 357 stability professionals. Over 60% had seen at least one product recall in the past five years. The biggest cause? Microbial growth in preservative systems.How does that happen? Water activity changes. If a cream absorbs moisture from the air, or if a liquid formulation loses water through evaporation, the preservative can become ineffective. Mold grows. Bacteria multiply. The product becomes unsafe.
It’s not just pharmaceuticals. Food industry experts have seen similar issues. One company extended the shelf life of its refrigerated soups by 22% by switching from basic USP methods to monitoring water activity and pH-tools that are now standard in food safety but rarely used in pharma.
And the stakes are rising. Climate change is making storage harder. A 2022 MIT study projected that by 2050, average drug shelf life could drop by nearly five months because warehouses in major distribution hubs will exceed 30°C for more than 87 days a year. That’s not hypothetical-it’s already happening in parts of the U.S., India, and Africa.
In low-income countries, nearly 30% of medicines fail stability tests due to poor supply chains. In high-income countries, it’s under 2%. That’s not a technical gap. It’s a systemic one.
What’s Changing-and What’s Not
There’s hope. The ICH Q12 guideline, effective since late 2023, allows companies to make post-approval changes to manufacturing or packaging without restarting full stability studies-so long as they can prove stability won’t be affected. This could speed up improvements.Companies like Amgen and Merck are using Risk-Based Predictive Stability (RBPS) models. These use data from multiple stress tests, machine learning, and real-time monitoring to predict degradation faster. In trials, they cut shelf-life determination time by 30%.
But regulatory agencies are slow to adopt them. The FDA and EMA still require years of real-time data for approval. Even though the science exists, the paperwork doesn’t keep up.
Meanwhile, the market is growing. The global stability testing industry is worth over $2.8 billion and will hit $4.1 billion by 2028. But most of that spending goes to big pharma. Smaller generic manufacturers can’t afford $1.2 million per product to run advanced stability programs.

What You Can Do
As a patient, you can’t test your pills. But you can protect yourself:- Store medications in a cool, dry place-not the bathroom or near the stove.
- Don’t use expired drugs, especially for critical conditions like heart disease or epilepsy.
- If your generic medication seems less effective, talk to your pharmacist. Ask if there’s a different manufacturer.
- Check for recalls. The FDA posts them online. If your drug was recalled for stability issues, stop using it.
Stability testing is invisible-but it’s the reason your medicine still works. It’s not just science. It’s safety. And for generics, that safety isn’t guaranteed just because the price is low.
How long do generic drugs really last after their expiration date?
Expiration dates are not arbitrary-they’re the last day the manufacturer guarantees full potency and safety under labeled storage conditions. While some drugs may remain chemically stable past this date, there’s no guarantee. Physical changes like crumbling, discoloration, or odor shifts mean the drug is no longer safe to use. For critical medications like insulin, nitroglycerin, or antibiotics, using expired versions can be dangerous.
Why do some generic drugs have shorter shelf lives than brand-name ones?
It’s usually because of differences in inactive ingredients, packaging, or manufacturing processes. Brand-name drugs often use proprietary coatings, moisture barriers, or stabilizers that generics can’t replicate without redeveloping the entire formulation. Even small changes in the binder or filler can affect how moisture or oxygen penetrates the tablet. That’s why a generic version of the same drug might have a 12-month shelf life while the brand lasts 36 months.
Can I trust the expiration date on my medication?
Yes-if the drug has been stored properly. The expiration date is based on real-time stability testing conducted under controlled conditions. If your medicine was kept in a hot car, a humid bathroom, or exposed to direct sunlight, it may degrade faster. Always check for visible changes: pills that are cracked, discolored, or smell odd should be discarded. Liquid medications that look cloudy or have particles should never be used.
Are there any drugs that become toxic when they degrade?
Yes. Tetracycline antibiotics degrade into toxic compounds that can damage the kidneys. Nitroglycerin breaks down into less effective forms and can fail to relieve angina during a heart attack. Some formulations of insulin can form aggregates that trigger immune reactions. Even common pain relievers like aspirin can break down into acetic acid and salicylic acid-while not highly toxic, they can irritate the stomach lining and reduce effectiveness.
How do regulators ensure generic drugs are stable?
Regulators require generic manufacturers to submit stability data showing their product performs similarly to the brand-name drug under the same storage conditions. But the testing protocols aren’t always as thorough. The FDA inspects facilities and reviews data, but oversight varies. Companies must follow ICH Q1A(R2) guidelines, but enforcement depends on resources. That’s why some generics pass initial testing but fail later-especially if they’re stored improperly before reaching the patient.


Wow, I never thought about how humidity in my bathroom could wreck my thyroid meds. Just moved all my pills to a drawer. Small change, big difference.
This is the most important post I’ve read all year. I work in a pharmacy and see people taking expired antibiotics like it’s no big deal. That tetracycline degradation point? Scary. We need more public education on this.
Let’s be real-generic manufacturers cut corners because they can. The FDA’s oversight is a joke. I’ve seen tablets from the same batch with different colors. If you’re on a life-saving drug, pay the extra $10. It’s not greed, it’s survival.
People who use expired meds are just irresponsible. If you can’t afford your prescription, ask for help-not to gamble with your life. I’ve seen too many overdoses from degraded drugs. Stop being lazy.
Just wanted to add: if you’re storing meds in a hot car or a humid bathroom, you’re not just risking potency-you’re risking your life. I’m a nurse, and I’ve seen patients end up in the ER because they thought ‘it’s probably still good.’ It’s not.
Imagine if your car’s brakes degraded slowly over time and no one told you. That’s what’s happening with your meds. The system is broken. Big pharma gets away with it because they have lobbyists. Generic makers? They’re stuck between a rock and a hard place-cheap ingredients, tight deadlines, zero room for error. And patients pay the price. I’m not mad, I’m just… heartbroken.
While I appreciate the technical depth of this post, I must emphasize that regulatory compliance must be held to the highest standard, regardless of cost. The ICH Q12 framework is a step forward, but without mandatory real-time environmental monitoring during distribution, we are merely delaying inevitable failures. Transparency and traceability are non-negotiable in pharmaceutical safety.