Getting vaccinated while on immunosuppressants isn’t just about popping a shot and moving on. It’s a high-stakes balancing act. Too early, and the vaccine might not stick. Too late, and you’re left vulnerable while your body’s defenses are down. For people on drugs like rituximab, methotrexate, or TNF inhibitors, the difference between protection and illness can come down to weeks-or even months.
Why Timing Matters More Than You Think
Immunosuppressants don’t just calm down inflammation-they mute your immune system’s ability to respond to threats. That’s good if you have rheumatoid arthritis or are recovering from a transplant. But it’s a problem when your body needs to build immunity from a vaccine. If you get vaccinated while your immune system is suppressed, you might not make enough antibodies. That means you’re not protected, even if you got the shot. Studies show that people on certain immunosuppressants can have up to 50% lower antibody levels after vaccination compared to healthy people. For mRNA vaccines like Pfizer and Moderna, that’s not just a small drop-it’s the difference between being shielded and being at risk. The CDC, ACR, IDSA, and ASH all agree: timing isn’t optional. It’s the most important factor in making vaccines work for immunocompromised people.When to Get Vaccinated Before Starting Immunosuppressants
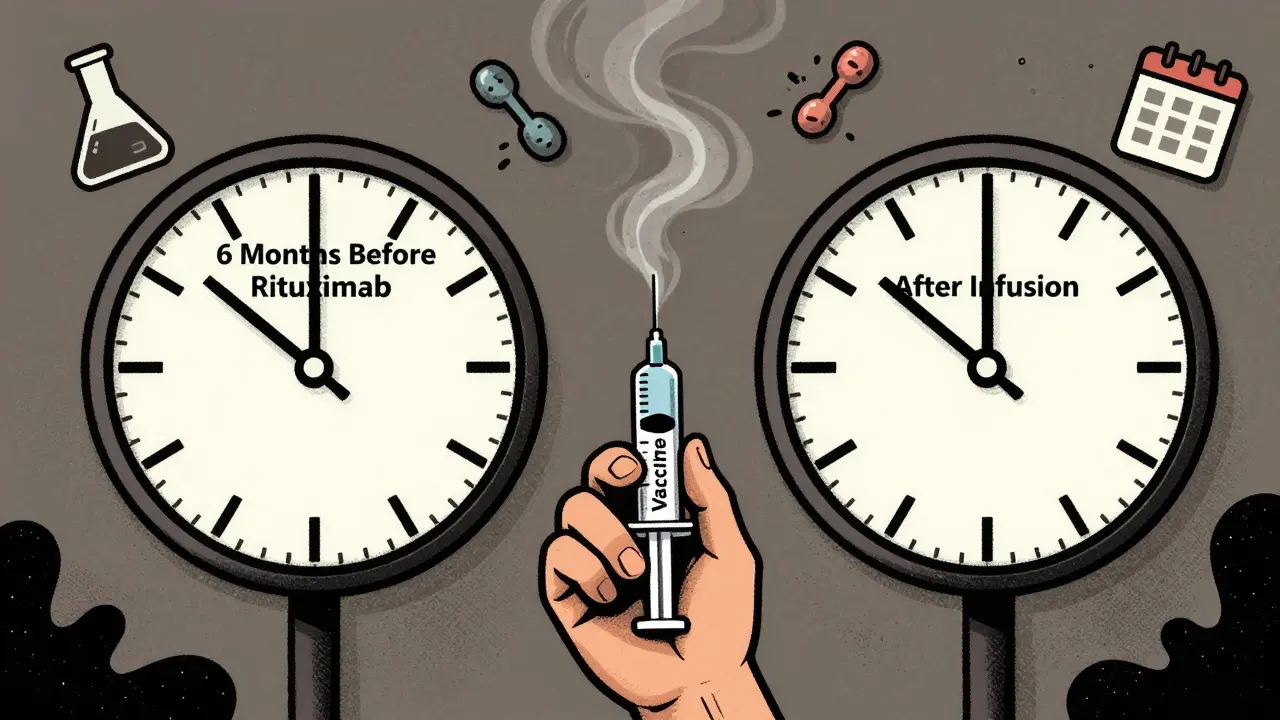
The best time to get vaccinated is before you even start taking immunosuppressants. All major guidelines agree on this. The CDC recommends at least 14 days before starting. But many specialists say that’s the bare minimum. For most people, aiming for 4 weeks before starting therapy gives the immune system the best shot. That’s especially true for vaccines like shingles (Shingrix), pneumococcal (Prevnar 20), and hepatitis B. If you’re scheduled to start rituximab, for example, you need to get all your vaccines at least 6 months before your first dose. Why? Because rituximab wipes out B-cells-the very cells that make antibodies. Once they’re gone, it takes months for them to come back. If you’re on long-term drugs like azathioprine or mycophenolate, you don’t need to stop them before inactivated vaccines (like flu or tetanus). But if you’re getting a live vaccine-like the old shingles shot (Zostavax) or MMR-you’ll need to pause these medications for at least 4 weeks before and after. Live vaccines can be dangerous if your immune system can’t control them.What to Do If You’re Already on Immunosuppressants
If you’re already taking immunosuppressants, it’s not too late-but you need to be smart about it. For drugs like methotrexate, holding the dose for two weeks after your flu shot can boost your antibody response by nearly 30%. That’s backed by three separate clinical trials. Many rheumatologists now recommend this as standard practice if your arthritis isn’t flaring. TNF inhibitors (like Humira or Enbrel) should be paused for one dose cycle before vaccination and restarted four weeks after. This small delay can make a big difference. A 2023 study in Annals of the Rheumatic Diseases found that patients who followed this timing had twice the chance of developing protective antibody levels compared to those who didn’t. Rituximab is the trickiest. Because it destroys B-cells, vaccines given within 6 months of your last dose often fail. The American College of Rheumatology says wait at least 6 months after your last infusion before getting any non-flu vaccine. But here’s the catch: if you’re in the middle of a flu outbreak, some experts say getting the shot sooner-even if it’s less effective-is better than waiting. It’s a risk-reward call, and it needs to be made with your doctor.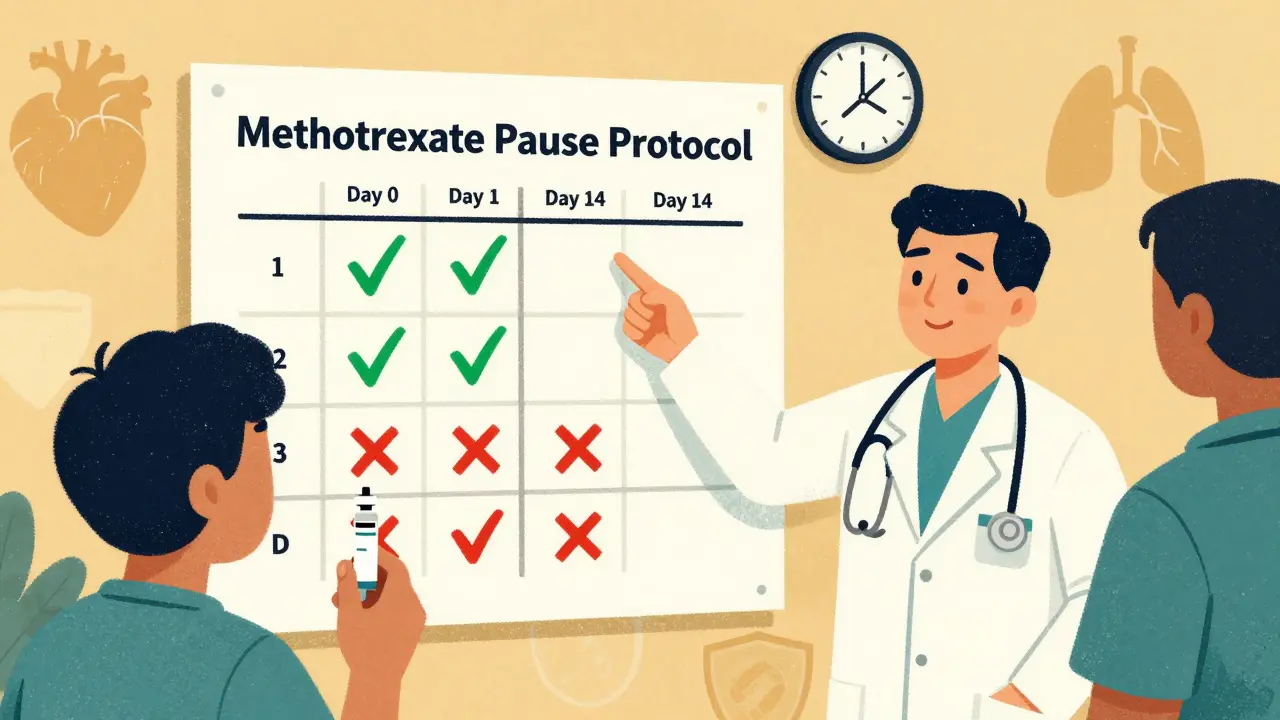
Special Cases: IVIG, Cyclophosphamide, and More
If you’re on IVIG (intravenous immunoglobulin), timing gets even more complicated. IVIG contains antibodies from donors, and those can interfere with live vaccines. For a 400 mg/kg dose, you need to wait 8 months before getting a live vaccine. For 2,000 mg/kg? You need to wait 11 months. After the vaccine, hold IVIG for 4 weeks. Cyclophosphamide is another beast. If you’re getting it as an IV infusion, you need to pause it for one cycle before vaccination and wait 4 weeks after to restart. Oral cyclophosphamide? Same rule. The key is avoiding vaccination during the nadir-the lowest point of your white blood cell count-which usually hits 7-14 days after the dose. Leflunomide and mycophenolate don’t need to be stopped for non-live vaccines, but they can dampen your response. If you’re on one of these and need a critical vaccine (like COVID-19 or hepatitis B), your doctor might consider a higher-dose version or an extra booster.Why Guidelines Clash-and What to Do About It
You’ll find contradictions if you read guidelines from different groups. The CDC says 14 days before immunosuppressants. ASH says 2-4 weeks. IDSA says 3 months after B-cell therapy. EULAR in Europe says 7-10 days for biologics. Which one do you follow? The truth? You follow the most conservative one that applies to your specific drug and condition. If you’re on rituximab, ignore the 14-day rule. Wait 6 months. If you’re on methotrexate and getting a flu shot, hold it for two weeks. Don’t guess. Don’t assume your doctor knows all the nuances-bring the guidelines with you. A 2023 survey of rheumatologists found that 68% struggle to apply these guidelines consistently. That’s why tools like the UCSF Immunossuppressant-Vaccine Timing Calculator were created. It’s free, online, and lets you plug in your meds and get a personalized window. Use it. Print it. Bring it to your appointment.Real-Life Consequences of Getting It Wrong
One patient in Massachusetts waited 6 months after her last rituximab dose to get the shingles vaccine. She got shingles during that window. Another, on methotrexate, skipped holding the drug before his flu shot. He still got the flu-and ended up in the hospital. But there are wins, too. A cancer survivor in Hamilton started his flu shot three weeks before chemo. He’s gone three years without a single respiratory infection. His oncologist timed it perfectly. The difference? Planning. Communication. Following the science, not the convenience.
What’s Coming Next: Personalized Timing
The future isn’t about fixed dates. It’s about measuring your immune system. New research from the NIH’s VAXIMMUNE study is testing whether checking your B-cell count (above 50 cells/μL) or antibody levels before vaccination is better than waiting 6 months. Early results suggest it is. If your B-cells are back, you’re likely ready for the vaccine-even if it’s been only 3 months since your last rituximab dose. Epic Systems is rolling out a new module in 2025 that will automatically flag when you’re due for a vaccine based on your meds. Your EHR will tell your doctor: “Patient on rituximab-last dose 4 months ago-B-cell count pending. Recommend vaccination in 2 weeks.” That’s the future. But right now, you still need to be your own advocate.What You Can Do Today
1. Make a list of every medication you’re on-including doses and last administration dates. 2. Know which are live vs. inactivated vaccines. Flu shot? Inactivated. Shingrix? Inactivated. MMR? Live. Zostavax? Live (but no longer used in the U.S.). 3. Check your last vaccine dates. Did you get pneumococcal in the last 5 years? Tetanus in the last 10? 4. Bring your meds and vaccine history to your next appointment. Don’t assume your doctor remembers everything. 5. Use the UCSF calculator (search: UCSF immunosuppressant vaccine timing tool). 6. Ask your doctor: “Should I hold any meds before or after my next vaccine?” If they say “I don’t know,” ask for a referral to an infectious disease specialist.When to Call Your Doctor Immediately
- You’re scheduled for a live vaccine and are on any B-cell depleting drug. - You’ve had a recent infection and are due for a vaccine. - You’re about to start a new immunosuppressant and haven’t been vaccinated in the past year. - You’re unsure whether your vaccine is live or inactivated. Don’t wait for symptoms. Don’t hope it’ll be fine. Immunocompromised people don’t get second chances.Can I get the flu shot while on methotrexate?
Yes, but you’ll get a better immune response if you hold methotrexate for two weeks after the shot. This is backed by clinical trials showing a 27% increase in antibody production. Only do this if your arthritis is stable-never if you’re having a flare. Always check with your rheumatologist first.
How long after rituximab should I wait for a vaccine?
Wait at least 6 months after your last rituximab infusion before getting any non-flu vaccine. For the flu shot, some experts say 3 months may be acceptable if community transmission is high. But for shingles, pneumococcal, or COVID boosters, stick to 6 months. B-cells need time to rebuild, and vaccines given too early often don’t work.
Are live vaccines safe if I’m on immunosuppressants?
Generally, no. Live vaccines like MMR, varicella, and the old Zostavax can cause infection in people with suppressed immune systems. Even if you’re not on strong drugs, avoid them unless your doctor says it’s safe. Shingrix is not live-it’s safe for most immunocompromised people. Always confirm the vaccine type before getting it.
Do I need extra doses of vaccines if I’m immunosuppressed?
Yes. The CDC recommends additional doses for COVID-19, hepatitis B, and pneumococcal vaccines in immunocompromised people. For example, you might need a 3-dose primary series for Pfizer/Moderna instead of 2. Ask your doctor if you’re due for extra shots. Many people don’t realize they’re eligible.
Can I get vaccinated while on IVIG?
You can get inactivated vaccines while on IVIG, but live vaccines are risky. If you need a live vaccine, you must wait: 8 months after a 400 mg/kg IVIG dose, 10 months after 1,000 mg/kg, and 11 months after 2,000 mg/kg. After the vaccine, pause IVIG for 4 weeks. These are strict rules-don’t skip them.