Potassium Intake Calculator
Why This Matters
When taking ACE inhibitors, your kidneys have reduced ability to remove potassium from your body. High potassium levels (hyperkalemia) can cause dangerous heart rhythm problems. This calculator helps you stay safely within recommended potassium limits based on your kidney function and health conditions.
Your Information
Recommended Daily Limit
Based on your kidney function, age, and health conditions, this is the maximum safe daily potassium intake to prevent hyperkalemia while taking ACE inhibitors.
Add Foods to Your Meal
Your Meal
Your Potassium Intake
Important Notes
Hyperkalemia Warning: Potassium levels above 5.0 mmol/L can cause dangerous heart rhythms. If you experience muscle weakness, fatigue, or irregular heartbeat, contact your doctor immediately.
Hidden Potassium: Salt substitutes, protein powders, and some medications contain potassium chloride, which can raise levels dangerously. Avoid these while on ACE inhibitors.
Regular Monitoring: Get your potassium checked regularly, especially after starting an ACE inhibitor or changing your dose.
When you’re taking an ACE inhibitor for high blood pressure, heart failure, or kidney disease, you’re doing something good for your heart. But there’s a quiet risk hiding in plain sight: your food. Some of the healthiest foods you eat-bananas, potatoes, spinach, avocados-can push your potassium levels too high. And when that happens while you’re on an ACE inhibitor, it can lead to hyperkalemia, a dangerous spike in blood potassium that can cause irregular heartbeat, muscle weakness, or even cardiac arrest.
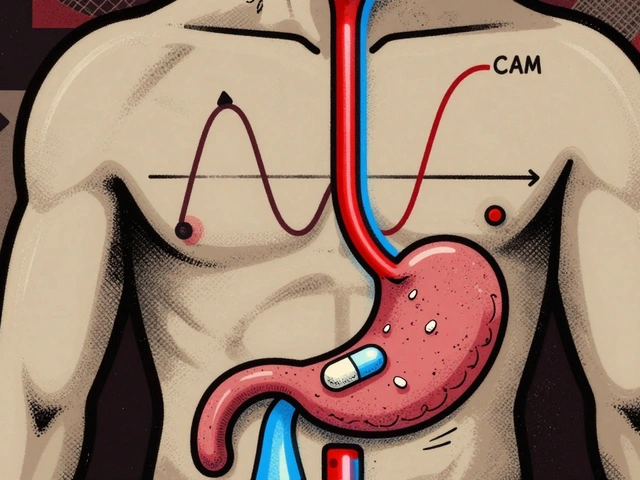
Why ACE Inhibitors Raise Your Potassium
ACE inhibitors work by blocking a hormone system called RAAS. This system normally tells your kidneys to release aldosterone, a hormone that helps your body get rid of extra potassium. When ACE inhibitors shut down aldosterone, potassium doesn’t get flushed out. It builds up in your blood. Studies show that within 24 hours of starting an ACE inhibitor, aldosterone drops by 40% to 60%. That means your kidneys lose their main tool for removing potassium.This isn’t just a minor side effect. About 1 in 5 people on ACE inhibitors develop hyperkalemia. The risk jumps even higher if you have kidney disease, diabetes, are over 75, or take other medications like potassium-sparing diuretics or certain antibiotics. In fact, people with an eGFR below 60 have more than three times the risk of dangerous potassium levels compared to those with healthy kidneys.
Which Foods Are the Biggest Risks?
You don’t need to give up healthy eating-but you do need to know which foods pack the most potassium. Here are the top offenders:- One medium banana: 422 mg
- One baked potato with skin: 926 mg
- One cup cooked spinach: 839 mg
- One medium tomato: 292 mg
- One avocado (1 cup sliced): 708 mg
- One cup orange juice: 496 mg
- One cup cooked lentils: 731 mg
- One cup coconut water: 1,150 mg
- One sweet potato (medium): 542 mg
These numbers aren’t just guidelines-they’re red flags. If your kidneys aren’t working well, even one or two of these foods a day can push your potassium over the safe limit. The National Kidney Foundation recommends keeping daily potassium under 2,000 mg if your eGFR is below 45. That’s less than half the amount many healthy adults consume.
Hidden Sources of Potassium
Many people think they’re eating clean and low-sodium, but they’re not watching potassium. Protein powders labeled “natural” or “plant-based” often have added potassium salts. Salt substitutes like NoSalt or Nu-Salt replace sodium chloride with potassium chloride-so one teaspoon can add over 800 mg of potassium. That’s more than two bananas in one spoonful.Processed foods aren’t always safe either. Some canned soups, frozen meals, and even bottled waters now contain potassium chloride as a preservative or flavor enhancer. Always check the ingredient list. If you see “potassium chloride,” “potassium citrate,” or “potassium phosphate,” it’s a warning sign.
One Reddit user on r/kidneydisease shared how they ended up in the ER after drinking 16 ounces of coconut water daily because they thought it was a “healthy hydration” choice. It contained over 1,150 mg of potassium. On lisinopril, that was enough to trigger a dangerous spike.
What You Can Eat Instead
You don’t have to eat bland food. There are plenty of low-potassium options that still taste good:- Apples, berries, grapes, pineapple
- Cabbage, green beans, zucchini, lettuce
- Rice, pasta, white bread
- Chicken, turkey, fish (in moderation)
- Egg whites
- White rice noodles
- Plain popcorn (no salt or butter)
Even better, you can reduce potassium in some high-potassium foods by leaching. For example, cut potatoes into thin slices, soak them in warm water for at least two hours, then rinse and boil them in plenty of water. This can cut potassium by up to 50%. The same works for carrots, beets, and winter squash. It’s a small effort for a big safety gain.
Monitoring and Testing
Your doctor should check your potassium and kidney function before you start an ACE inhibitor-and again within 7 to 14 days after starting or changing your dose. After that, testing every 3 to 4 months is standard. If your creatinine rises by more than 30% or your potassium goes above 5.0 mmol/L, your dose may need to be lowered or changed.Don’t wait for symptoms. Hyperkalemia often has none-until it’s too late. Some people feel muscle cramps, fatigue, or a strange heartbeat, but many feel nothing. That’s why regular blood tests aren’t optional. They’re your early warning system.
Medications That Make It Worse
Some common drugs can team up with ACE inhibitors to push potassium even higher:- Potassium-sparing diuretics (spironolactone, eplerenone, triamterene)
- Trimethoprim/sulfamethoxazole (Bactrim)
- NSAIDs like ibuprofen or naproxen
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Some herbal supplements (like licorice root)
Combining ACE inhibitors with spironolactone increases hyperkalemia risk by over 50%. That’s why many doctors now avoid this combo unless absolutely necessary-and even then, they monitor closely. If you’re on any of these, talk to your doctor about alternatives. For example, instead of Bactrim for a UTI, they might prescribe nitrofurantoin, which doesn’t affect potassium.
New Tools to Help You Stay Safe
There’s good news: new tools are making it easier to manage this risk. Potassium binders like patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) can pull excess potassium out of your gut before it enters your bloodstream. Clinical trials show these drugs reduce the chance of stopping your ACE inhibitor due to high potassium by 41%.They’re not magic pills-they cost money, need to be taken daily, and can cause constipation or diarrhea. But for people who need ACE inhibitors to survive, they’re a game-changer. The American Heart Association now recommends them for high-risk patients who can’t tolerate dietary changes alone.
Apps like Renal Diet Helper and MyKidneyCoach let you scan food labels and track potassium intake. One study found that patients who used these tools were 34% less likely to have a dangerous potassium spike than those who just got printed handouts.
What to Do If You’re at Risk
If you’re on an ACE inhibitor and have kidney disease, diabetes, or are over 75, here’s your action plan:- Get your potassium and eGFR checked before starting and again 7-14 days after starting.
- Ask your doctor for a personalized potassium limit-usually under 2,000 mg/day if your kidneys are impaired.
- Get a laminated food chart from your dietitian showing low- and high-potassium options.
- Use a potassium-tracking app daily for the first month to build awareness.
- Avoid salt substitutes and potassium-containing supplements.
- Ask your pharmacist to review all your medications for hidden potassium risks.
- Call your doctor immediately if you feel heart palpitations, muscle weakness, or extreme fatigue.
Don’t stop your ACE inhibitor unless your doctor tells you to. The benefits for your heart and kidneys usually outweigh the risks-especially when you’re careful.
Final Thought: Knowledge Is Your Shield
A 2023 review found that patients who understood their potassium risks were 57% less likely to develop hyperkalemia. That’s not because they were perfect. It’s because they knew what to watch for. You don’t need to become a nutritionist. You just need to know which foods are risky, how to check your levels, and when to speak up.Your ACE inhibitor is helping you live longer. Don’t let a banana or a cup of coconut water undo that. Stay informed. Stay tested. Stay safe.
Can I still eat bananas if I’m on an ACE inhibitor?
You can eat bananas occasionally if your kidney function is normal and your potassium levels are stable. But if you have kidney disease, diabetes, or are over 75, even one banana a day can push your potassium too high. Talk to your doctor or dietitian about your personal limit. For many, it’s best to avoid them entirely or eat them only once a week in small portions.
How do I know if my potassium is too high?
You won’t always feel it. Early signs can be subtle: muscle weakness, fatigue, irregular heartbeat, or nausea. But many people have no symptoms at all until it becomes dangerous. The only reliable way to know is through a blood test. If you’re on an ACE inhibitor, get your potassium checked regularly-especially after starting the medication or changing your dose.
Is it safe to use salt substitutes on an ACE inhibitor?
No. Most salt substitutes replace sodium with potassium chloride. One teaspoon can contain over 800 mg of potassium-more than two bananas. For someone on an ACE inhibitor with reduced kidney function, that’s enough to trigger a dangerous spike. Use herbs, lemon juice, or no-salt seasoning blends instead.
Can I take potassium supplements while on an ACE inhibitor?
Absolutely not-unless your doctor specifically prescribes it, which is rare. Most people on ACE inhibitors are already at risk of high potassium. Taking extra potassium, even in a multivitamin, can be life-threatening. Always check the label of any supplement for potassium content.
What should I do if I miss a dose of my ACE inhibitor?
Take it as soon as you remember, unless it’s almost time for your next dose. Don’t double up. Missing one dose won’t suddenly cause hyperkalemia, but skipping doses regularly can make your blood pressure harder to control. Always talk to your doctor before changing your dosing schedule.
Are there any new medications that help prevent hyperkalemia?
Yes. Drugs like patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) bind potassium in your gut and remove it from your body. They’re not first-line treatments, but they’re a big help for people who need to stay on ACE inhibitors but keep developing high potassium. These medications have been shown to reduce the need to stop ACE inhibitor therapy by over 40%.
If you’re on an ACE inhibitor, you’re managing a chronic condition-and that takes daily awareness. You don’t need to live in fear. You just need to be informed. Know your numbers. Know your food. Know your limits. And never be afraid to ask your doctor or dietitian for help. Your heart is worth it.



Man, I never thought about how something so simple as a banana could be a silent killer when you're on ACE inhibitors. It's wild how medicine and food are so deeply intertwined. I used to think 'healthy eating' meant just loading up on fruits and greens - turns out, for some of us, that's the exact opposite of safe. This post made me reevaluate everything I thought I knew about nutrition and chronic illness. We need more of these real-talk breakdowns.
As a renal dietitian I see this all the time. People think coconut water is 'nature's Gatorade' - it's not. It's potassium in a bottle. I hand out laminated lists to every patient starting ACEi. And yes, leaching potatoes works - I've seen people drop their K+ by 0.8 mmol/L just by soaking them. Don't skip the blood tests. Your heart doesn't care how 'clean' your diet is.
bro i was drinking 2 coconuts a day thinking i was being healthy 😭 then my doc was like 'you're lucky you didn't code' and i was like... wait what? i thought potassium was good?? like why are we punishing avocados?? this is insane. i switched to apples and now i just stare at my banana like it's a traitor. also i got a veltassa script now and it's kinda gross but i'll take it over a heart attack 🙏
Wow. Another overblown fearmongering article from the medical-industrial complex. You're telling me people can't eat fruit because they're on a drug? Maybe the drug is the problem, not the food. Also, 2000mg limit? That's lower than what some African tribes consume daily. This is just another way to make people dependent on expensive binders and tests. Wake up.
As someone who moved from India to the US and now manages hypertension with lisinopril, I can say this: the cultural shift in diet is real. Back home, we ate rice, lentils, and greens - low potassium. Here, everyone’s on avocado toast and smoothies. I had to relearn everything. I now use MyKidneyCoach daily. It’s not perfect, but it’s saved me from three ER visits. Don’t let pride stop you from tracking. Your body will thank you.
yo so like ACEi inhibits RAAS which downregulates aldosterone which reduces k+ excretion - basic pharmacology. but ppl dont get that potassium isn't 'bad' it's just that if your GFR is <60 your kidneys are already struggling so adding 1150mg from coconut water is like pouring gasoline on a candle. also salt substitutes? bro that's just potassium chloride. you think you're being healthy but you're just doing a slow suicide. check your med list. if it has 'chloride' in it - skip it.
THIS. IS. EVERYTHING. 🙌 I was on spironolactone + lisinopril and didn’t realize it was a combo of doom. My hands were shaking, I felt like I was underwater - thought it was stress. Turned out my K+ was 6.1. I almost died. Now I eat white rice, chicken, and apples. I even boil my potatoes. I’m alive because I read this. THANK YOU. 🥹❤️
Oh great. So now I can’t eat anything that’s not white and bland? I’m supposed to give up spinach and sweet potatoes because some doctor said so? What’s next? No breathing because oxygen might cause a spike? This is just medical gaslighting wrapped in a food chart. You know what’s dangerous? Trusting Big Pharma’s new $500/month potassium binder instead of fixing the root cause. 🙄
Let’s be real - the real issue here is that physicians don’t adequately educate patients before prescribing ACE inhibitors. You’re handing someone a drug with a 20% hyperkalemia risk and saying ‘eat healthy’ without teaching them what that means. It’s negligence. The fact that apps like Renal Diet Helper even exist proves the system failed. The burden shouldn’t be on the patient to become a nutritionist to stay alive.
I’ve been on lisinopril for 8 years. I eat one banana a week, no salt substitutes, and I boil my potatoes. I check my labs every 3 months. It’s not hard. You don’t need to be perfect. You just need to be aware. This post saved me from a bad habit I didn’t even know I had. Thanks for the clarity.
It’s not about fear. It’s about balance. Your kidneys are your filters. If they’re weak, you can’t dump potassium like before. That’s biology, not conspiracy. You don’t have to give up food. You just have to know what’s safe. Simple.
Who’s behind this? Big Pharma? The FDA? The American Heart Association? They all profit from these ‘dangerous potassium’ scares. Why not just tell people to stop taking ACE inhibitors? Oh right - because they’re billion-dollar drugs. And now you need a $500/month binder to keep taking them. Classic. I’m not eating any of this. Literally or figuratively.
It’s fascinating how we’ve turned food into a moral test. We’re not punishing people for eating - we’re helping them survive. I’ve seen patients who refused to change their diet and ended up in dialysis. Knowledge isn’t control. It’s freedom. And yes, leaching potatoes works - I’ve done it with my mom. It’s tedious, but it’s worth it.
Just read the comment from Andrea DeWinter - she’s right. Leaching potatoes? I never knew that. I’ve been boiling them like normal. So I just cut them thin, soak for two hours, rinse, then boil again? That’s… actually doable. I’m trying it this weekend. Also, I’m deleting my coconut water app. I’m officially a banana exile now. 😅