Drug Interaction Calculator
Amiodarone-Digoxin-Warfarin Calculator
This tool calculates safe dose adjustments and monitoring recommendations when combining amiodarone with digoxin and warfarin. Based on evidence from 2023 clinical guidelines.
Results
When three common heart medications are taken together, the result isn’t just a doubled effect - it’s a triple threat that can send patients to the ICU. Amiodarone, digoxin, and warfarin are each prescribed for serious heart conditions. But when they’re combined, their interactions don’t just add up - they multiply. This isn’t theoretical. It’s happening in hospitals, nursing homes, and living rooms across the country every single day.
Why This Triad Is So Dangerous
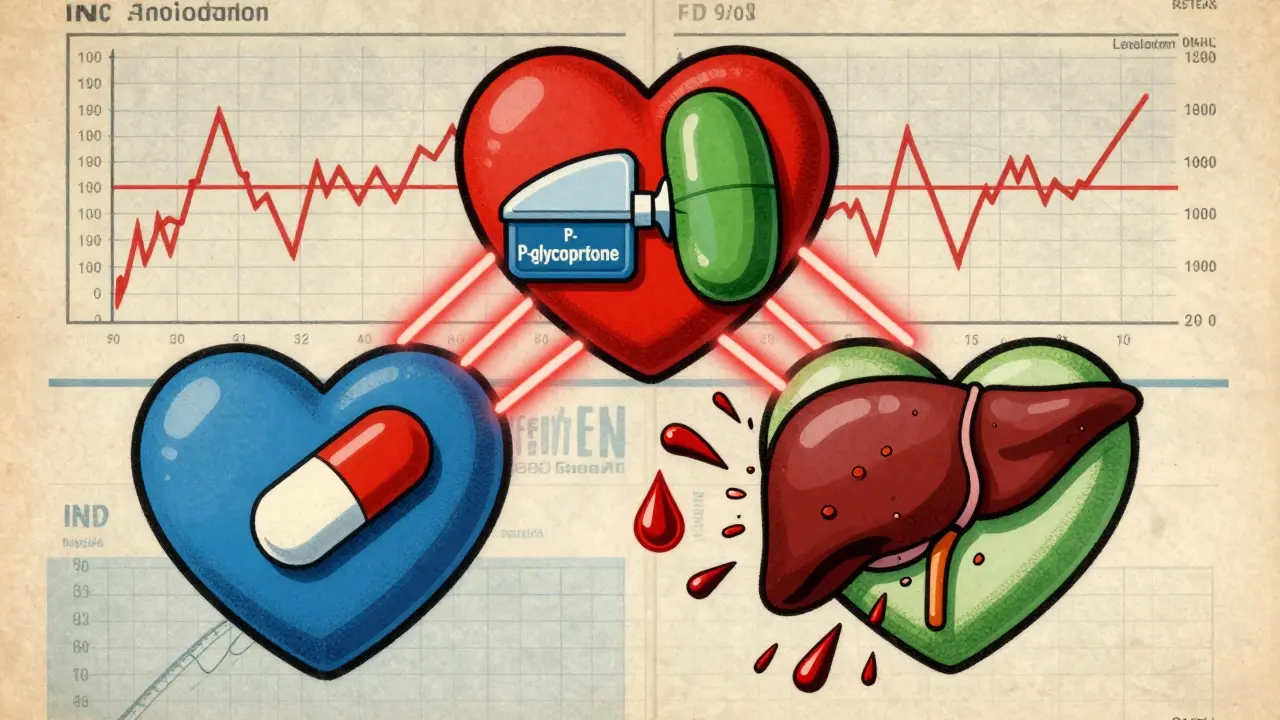
Amiodarone is a powerful antiarrhythmic used to treat irregular heartbeats like atrial fibrillation and ventricular tachycardia. Digoxin slows the heart rate in patients with heart failure or atrial fibrillation. Warfarin prevents dangerous blood clots. Individually, each drug works well. Together? They turn into a ticking time bomb. The real danger lies in how amiodarone messes with the body’s ability to clear the other two drugs. It doesn’t just slow things down - it nearly shuts them down. For digoxin, amiodarone blocks a key transporter called P-glycoprotein. This protein normally pushes digoxin out of the body through the kidneys and liver. When it’s blocked, digoxin builds up. Studies show serum levels can jump by 40% to 100% within just a week. That’s not a small change. Digoxin toxicity isn’t just nausea or dizziness - it can trigger deadly heart rhythms like ventricular tachycardia. In elderly patients, levels above 1.2 ng/mL are considered dangerous. With amiodarone, many patients cross that line without anyone realizing why. For warfarin, amiodarone does something even more insidious. It blocks the liver enzymes (CYP2C9 and CYP3A4) that break down warfarin. This means warfarin sticks around longer, and its anticoagulant effect skyrockets. The result? INR levels - the measure of blood thinning - can spike from a safe 2.5 to over 8 in a matter of days. An INR above 4 means your blood takes way too long to clot. Above 10? You’re at serious risk of internal bleeding. And here’s the kicker: digoxin can make warfarin’s effect even worse. High digoxin levels displace warfarin from protein binding sites, freeing up more active drug into the bloodstream. So you’ve got amiodarone boosting digoxin, and digoxin boosting warfarin. It’s a feedback loop of risk.What Happens When It Goes Wrong
The consequences aren’t abstract. They’re bloody, brutal, and often fatal. A 2021 study in Circulation: Arrhythmia and Electrophysiology looked at over 4,800 patients on amiodarone and digoxin. Those on both drugs had a 23% higher risk of death than those on digoxin alone. The biggest spike? In the first 30 days after starting amiodarone. Warfarin complications are even more terrifying. A 2020 study of nearly 13,000 patients found that those taking amiodarone alongside warfarin were 4.2 times more likely to have an INR over 4.0. Major bleeding risk jumped by 180%. One case from Massachusetts General Hospital involved a patient whose INR hit 12.4 after just 10 days on amiodarone. He needed four units of plasma and IV vitamin K to survive. The FDA’s Adverse Event Reporting System recorded over 1,800 cases of digoxin toxicity linked to amiodarone between 2010 and 2022. That’s a 5.3-fold increase compared to digoxin alone. And in 2022 alone, 387 deaths were tied to this exact combination - a 12% jump from the year before. Elderly patients are hit hardest. Many are on all three drugs because they have atrial fibrillation, heart failure, and a history of stroke. They’re also more sensitive to drug buildup. A 2022 study in JAMA Internal Medicine found that 63% of consultation requests about this triad came from patients over 75. Many had fallen, hit their head, and ended up with a brain bleed because their warfarin dose wasn’t adjusted.How to Survive This Triad - If You Must Take It
The truth? Many patients can’t avoid this combination. Atrial fibrillation often needs all three drugs. But you can survive it - if you know how to manage it. Step 1: Reduce digoxin before you even start amiodarone. The standard advice is to cut the digoxin dose by 50% right away. Don’t wait for symptoms. Don’t wait for lab results. If you’re starting amiodarone and already on digoxin, reduce it immediately. Then check the digoxin level 72 hours later. If it’s above 1.0 ng/mL, reduce further. Step 2: Halve your warfarin dose before adding amiodarone. This isn’t optional. A 2022 ACC update says to reduce warfarin by 30-50% before starting amiodarone. Then test your INR every 48 to 72 hours for the first two weeks. Weekly checks are not enough. You need daily or every-other-day monitoring. Step 3: Keep monitoring long after stopping amiodarone. This is where most providers fail. Amiodarone stays in your body for months. Its half-life? Up to 100 days. That means even after you quit taking it, your digoxin and warfarin levels are still being affected. The NHS recommends continuing INR checks for 4 to 6 weeks after stopping amiodarone. Some experts say up to 8 weeks for elderly patients. Step 4: Consider switching away from warfarin. Newer anticoagulants like apixaban or rivaroxaban (DOACs) don’t interact with amiodarone the same way. They’re not perfect - they still have some interaction with P-glycoprotein - but the risk is far lower. If you’re newly diagnosed with atrial fibrillation and need anticoagulation, DOACs are now the first choice for 82% of patients. But if you have a mechanical heart valve, you’re stuck with warfarin. That’s where the danger is highest.What’s Being Done - And What Still Needs to Change
Hospitals are catching on. A 2023 NHS England report showed that when hospitals implemented strict protocols - automatic dose reductions, EHR alerts, mandatory weekly INR checks - adverse events dropped by 78% across 47 hospital trusts. Electronic health records now have built-in alerts for this triad. A 2022 study found that hospitals using these alerts reduced prescribing errors by 65%. But not all systems are equal. Many still miss the warning if the patient is on a generic version of one drug. Or if the dose is low. Or if the patient is in a nursing home without a pharmacist on staff. Genetics are also changing the game. A 2023 study found that people with a specific gene variant (ABCB1 C3435T TT) had 92% higher digoxin levels when taking amiodarone. That’s not a small difference - it’s a life-or-death gap. We’re not testing for this routinely. But we should be.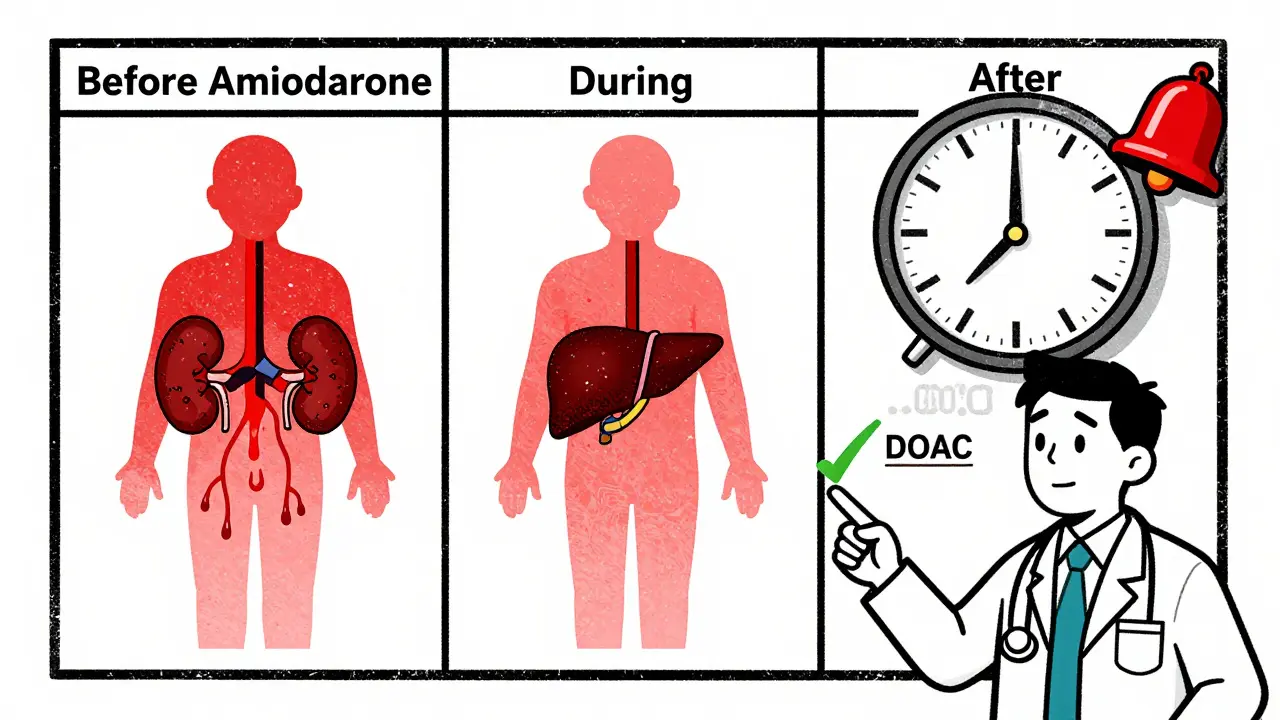
What Patients Need to Know
If you’re on all three of these drugs:- Know your digoxin level. Ask for it every time you refill.
- Know your INR. Don’t wait for your doctor to call. Check it yourself if you can.
- Watch for signs of digoxin toxicity: nausea, vomiting, blurred vision, seeing yellow or green halos around lights, or an irregular heartbeat.
- Watch for signs of bleeding: bruising without injury, nosebleeds, blood in urine or stool, headaches, dizziness, or weakness.
- Never change your dose on your own - but don’t be afraid to ask your pharmacist or doctor: “Is this safe with what I’m already taking?”
Final Reality Check
This triad isn’t rare. It’s common. The American Heart Association estimates 4.3 million Americans will still be on this dangerous combination by 2030. Why? Because many have mechanical heart valves. Because warfarin is cheaper. Because some patients can’t afford DOACs. The good news? This interaction is predictable. Preventable. Documented since 1983. The bad news? Too many providers still don’t know how to manage it. Too many patients are left in the dark. If you’re taking this trio, your life depends on one thing: awareness. Not just your awareness - your doctor’s, your pharmacist’s, your family’s. Because if no one is watching, this combination will kill you quietly.Can I take amiodarone with digoxin if I’m not on warfarin?
Yes, but it’s still risky. Even without warfarin, the amiodarone-digoxin interaction alone increases mortality risk by 23%. The 2018 DIG-Amio study showed that patients on both drugs had significantly higher death rates than those on digoxin alone. Always reduce the digoxin dose by at least 50% when starting amiodarone, and monitor serum levels closely.
How long does amiodarone affect digoxin and warfarin after I stop taking it?
Amiodarone has an extremely long half-life - between 25 and 100 days. That means its effects on digoxin and warfarin can last for weeks to months after you stop. Digoxin levels may stay elevated for 4-6 weeks. Warfarin’s effect can linger for up to 8 weeks. You must continue INR monitoring and digoxin level checks during this entire period. Never assume the interaction stops when you stop the drug.
Are there safer alternatives to this drug combination?
For anticoagulation, direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, or dabigatran are much safer with amiodarone than warfarin. For rate control, beta-blockers (like metoprolol) or calcium channel blockers (like diltiazem) are preferred over digoxin. But if you have a mechanical heart valve, you can’t use DOACs - and digoxin may still be needed. Talk to your cardiologist about your options - don’t assume you’re stuck with this triad.
What should I do if I start feeling dizzy or nauseous after starting amiodarone?
Don’t wait. Call your doctor or go to the ER immediately. Nausea, vomiting, blurred vision, or an irregular heartbeat could mean digoxin toxicity. If you’re also bruising easily, bleeding from your gums, or passing dark stools, it could mean warfarin overdose. Both are medical emergencies. Your INR and digoxin level need to be checked right away.
Is this interaction more dangerous in older adults?
Yes. Older adults have slower kidney and liver function, which means drugs clear more slowly. They’re also more sensitive to changes in digoxin and warfarin levels. Studies show 63% of consultation requests for this triad come from patients over 75. Falls, brain bleeds, and death are far more common in this group. Extra caution - and more frequent monitoring - is absolutely necessary.