When your blood sugar stays high for years, it doesn’t just affect your kidneys or nerves-it quietly damages the tiny blood vessels in your eyes. This is diabetic retinopathy, and it’s the leading cause of vision loss in working-age adults in the U.S. Many people don’t know they have it until their vision starts to blur, floaters appear, or they struggle to see at night. By then, it’s often too late to fully reverse the damage. But here’s the good news: if caught early, most vision loss from diabetic retinopathy can be prevented.
How Diabetes Turns Your Retina Into a Battlefield
Your retina is the light-sensitive layer at the back of your eye. It turns images into signals your brain understands. But when you have diabetes, high blood sugar slowly weakens the blood vessels that feed the retina. These vessels start to leak fluid, swell, or get blocked. Over time, the eye tries to fix itself by growing new blood vessels. But these new vessels are fragile. They bleed easily, scar the retina, and can even pull it away from the back of the eye-causing sudden, severe vision loss.This isn’t a fast process. It takes years. That’s why so many people with diabetes don’t notice anything wrong until the damage is advanced. The eye doesn’t hurt. There’s no redness. No swelling. Just a slow, silent decline in vision. According to the National Eye Institute, about 1 in 3 adults with diabetes will develop some form of retinopathy. And nearly 7% will develop diabetic macular edema-a specific type where fluid leaks into the macula, the part of the retina responsible for sharp central vision. That’s when reading, driving, and recognizing faces becomes hard.
The Three Stages of Retinal Damage
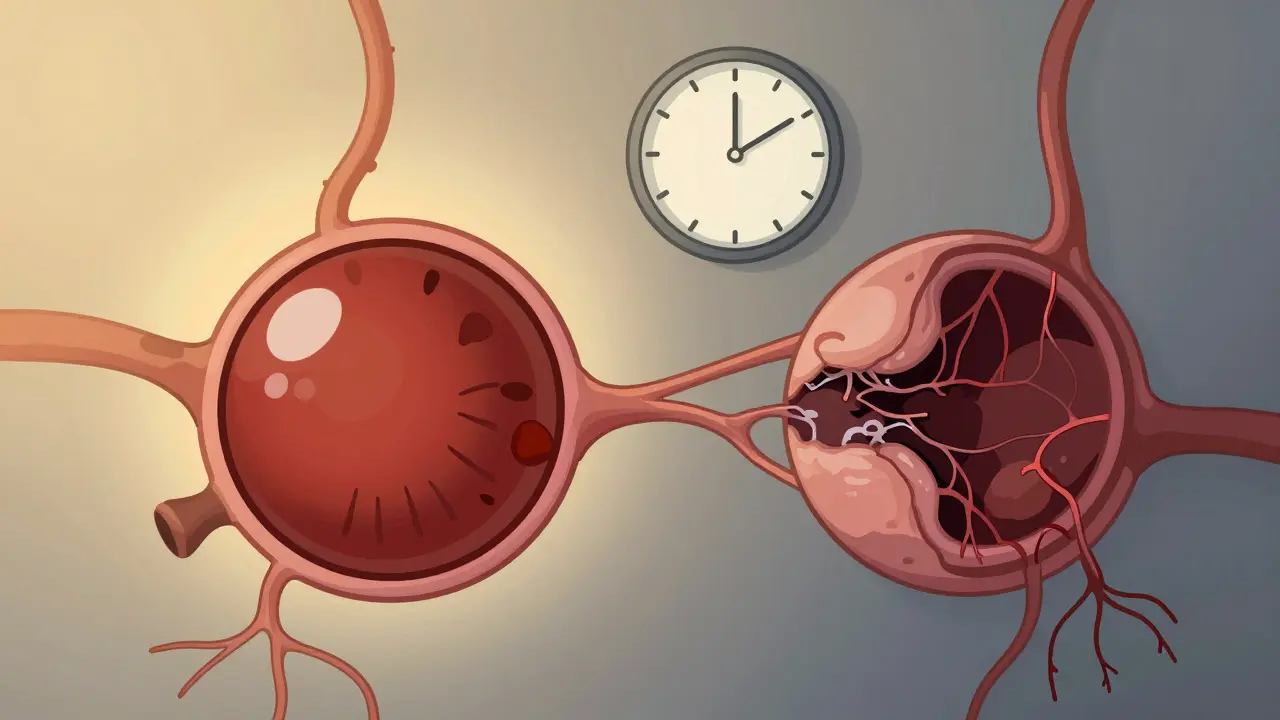
Diabetic retinopathy doesn’t happen all at once. It moves in clear stages:- Mild Nonproliferative Retinopathy: Tiny bulges called microaneurysms form in the blood vessels. These can leak small amounts of fluid. At this stage, you likely won’t notice any changes in your vision.
- Moderate to Severe Nonproliferative Retinopathy: More blood vessels become blocked. The retina starts to swell, and bleeding may occur. Vision may begin to blur, especially if fluid builds up in the macula.
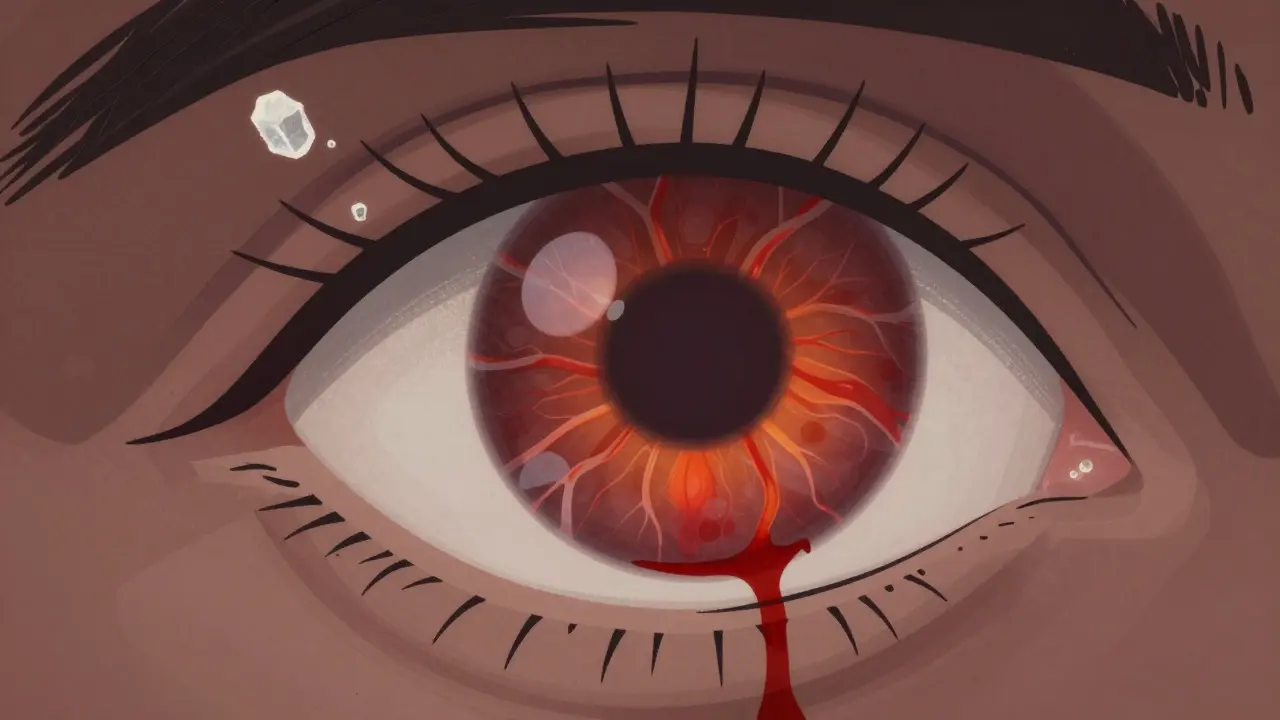
- Proliferative Diabetic Retinopathy: The retina, starved of oxygen, starts growing new blood vessels. These vessels are weak and messy. They bleed into the vitreous (the gel-like fluid inside your eye), causing floaters or sudden vision loss. They can also form scar tissue that pulls the retina loose-leading to retinal detachment, a medical emergency.
Diabetic macular edema can happen at any stage, but it’s most common in the moderate to severe stages. It’s not a separate disease-it’s a complication that makes vision worse faster.
Why You Can’t Rely on Symptoms
This is the hardest part for most people to accept: you can have serious retinal damage and still see perfectly. A study from the University Health’s Texas Diabetes Institute found that 68% of patients didn’t notice symptoms until the condition was already moderate or worse. That’s why waiting for blurry vision or floaters is a dangerous gamble.When symptoms do show up, they’re often subtle at first:
- Blurred or wavy vision (reported by 78% of patients in later stages)
- Floaters or dark spots floating across your vision (65% of cases)
- Difficulty seeing at night or in low light (52% of patients)
- Fading or washed-out colors (41% of cases)
- Loss of peripheral vision (37% of advanced cases)
Bleeding into the eye is often the first clear sign something’s wrong. But by then, the damage is already done. The only way to catch it early is through a yearly dilated eye exam. No exceptions.
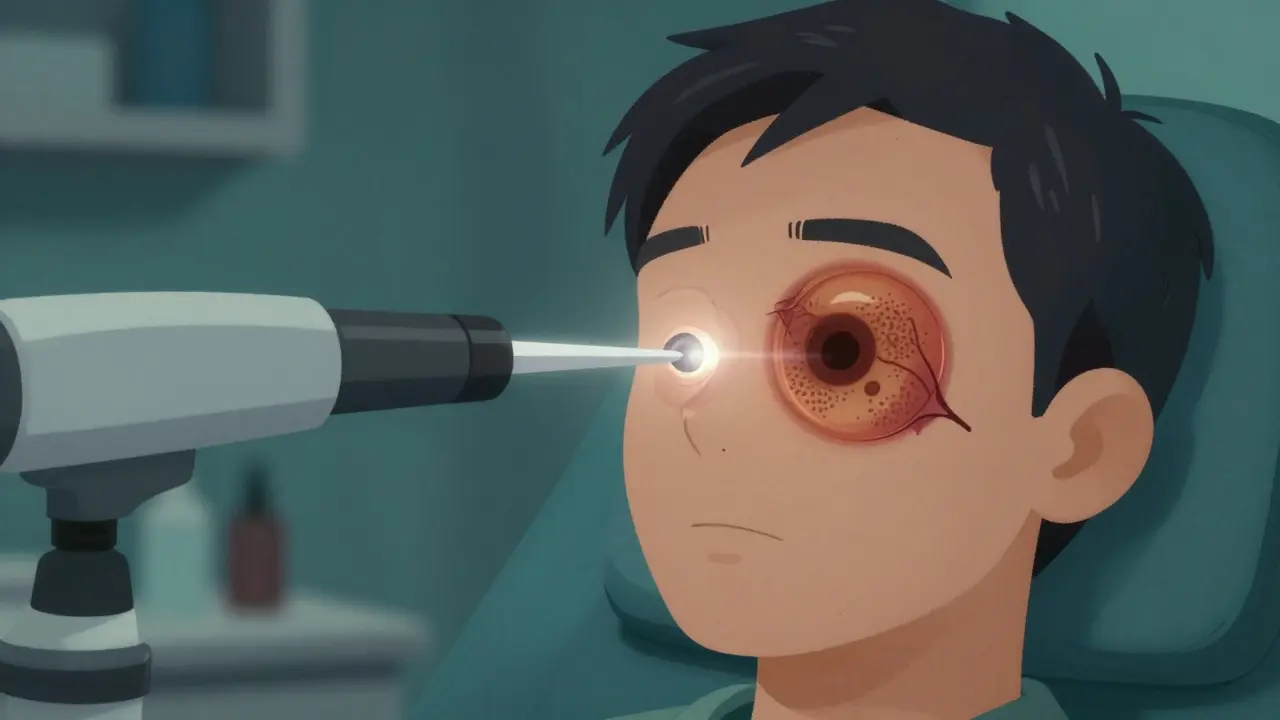
Laser Treatment: How It Stops the Damage
Laser treatment-called photocoagulation-has been the gold standard for treating advanced diabetic retinopathy for decades. It’s not a cure, but it’s highly effective at stopping progression.Here’s how it works: a focused beam of light is aimed at the damaged areas of the retina. The heat from the laser seals leaking blood vessels and shrinks abnormal new ones. It doesn’t restore lost vision, but it dramatically reduces the risk of further vision loss.
There are two main types:
- Focal laser treatment: Used for diabetic macular edema. The laser targets specific leaky vessels near the macula to reduce swelling.
- Scatter laser treatment (panretinal photocoagulation): Used for proliferative retinopathy. Hundreds of tiny laser burns are spread across the peripheral retina. This reduces the retina’s demand for oxygen, which stops the growth of abnormal new vessels.
The procedure is done in an outpatient clinic. You’ll get numbing eye drops. You might feel a slight stinging sensation, but it’s not painful. Most people go home the same day. Vision might be blurry for a few hours, and you’ll need someone to drive you home.
Success rates are strong: patients who get timely laser treatment have a 95% chance of preserving their vision, according to UVA Health. That’s not a guarantee you’ll see better-but it’s a near-certainty you won’t lose what you have.
It’s Not Just About the Laser
Laser treatment works best when paired with tight diabetes control. If your blood sugar stays high, the laser won’t stop the damage from coming back.Research from the Cleveland Clinic shows a direct link between your HbA1c levels (a measure of long-term blood sugar) and how fast retinopathy progresses. Keeping your HbA1c below 7% slows damage significantly. Lower is better-especially if you’re younger or have had diabetes for more than 10 years.
Other factors matter too:
- High blood pressure: Makes blood vessels more likely to leak. Keep it under 130/80.
- High cholesterol: Contributes to vessel blockages.
- Smoking: Damages blood vessels and speeds up retinopathy.
- Pregnancy: Can cause rapid worsening in women with diabetes.
Managing these isn’t optional. It’s part of the treatment plan.
What’s New? Beyond the Laser
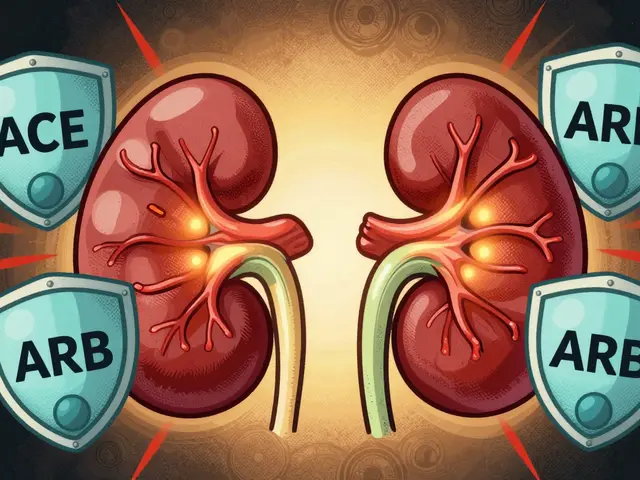
Laser treatment is still a cornerstone, but it’s no longer the only tool. In recent years, injections of anti-VEGF drugs-like ranibizumab and aflibercept-have become common. These medications block the signal that tells the eye to grow abnormal blood vessels. They’re especially effective for diabetic macular edema and can sometimes improve vision, not just stop it from getting worse.Many patients now get a combination: anti-VEGF shots first to reduce swelling, then laser to seal off the remaining leaky vessels. This approach is more effective than either treatment alone.
Research is also moving toward longer-lasting treatments and even gene therapies. But for now, laser remains reliable, affordable, and widely available.
What Happens If You Don’t Treat It?
Left untreated, diabetic retinopathy leads to irreversible damage. The retina can detach. Bleeding can fill the eye. Scar tissue can permanently distort vision. In advanced cases, blindness is common.It’s not just about losing sight. It’s about losing independence-driving, reading, recognizing faces, walking safely. The economic cost in the U.S. is estimated at hundreds of millions annually. But the human cost? Unmeasurable.
And here’s the hard truth: once photoreceptor cells (the light-sensing cells in your retina) die, they don’t come back. That’s why timing matters more than anything.
Your Action Plan
If you have diabetes, here’s what you need to do-right now:- Get a dilated eye exam every year. Even if your vision is perfect. If you’re pregnant or have existing retinopathy, you may need more frequent checks.
- Keep your HbA1c under 7%. Talk to your doctor about your target. Lower is better, but don’t risk low blood sugar to get there.
- Control your blood pressure and cholesterol. Medications, diet, and exercise all play a role.
- Quit smoking. If you smoke, get help. It’s one of the fastest ways to speed up eye damage.
- Don’t wait for symptoms. If you notice floaters, blurred vision, or trouble seeing at night, call your eye doctor immediately. Don’t wait for your annual checkup.
Diabetic retinopathy isn’t inevitable. It’s preventable. But prevention requires action-consistent action, year after year. Your eyes are watching you. Don’t make them wait until it’s too late.
Can diabetic retinopathy be reversed?
Early damage can be stabilized, but once photoreceptor cells die or scar tissue forms, the damage is permanent. Laser treatment and anti-VEGF injections can stop further vision loss and sometimes improve vision slightly, especially in cases of macular edema. But they can’t restore vision lost to long-term damage. That’s why early detection is everything.
Is laser treatment painful?
Most people feel only mild discomfort, like a quick pinch or pressure. Numbing drops are used, and the procedure takes less than 30 minutes. You might see flashes of light during the treatment, but it’s not painful. Afterward, your vision may be blurry for a few hours, and you’ll need someone to drive you home.
How often do I need laser treatment?
Many people need only one or two sessions, especially if caught early. But if your diabetes isn’t well controlled, new damage can develop over time. Some patients need repeat treatments every few months or years. Regular eye exams are the best way to know if more treatment is needed.
Can I still drive if I have diabetic retinopathy?
It depends on how much vision you’ve lost. If your central or peripheral vision is affected, driving may become unsafe. Your eye doctor will assess your vision and may report changes to your local licensing authority. Many people with early-stage retinopathy can still drive safely with regular treatment and monitoring.
Do I need to see a specialist?
Yes. While your regular eye doctor can do initial screenings, you’ll need to see a retinal specialist (a retina specialist or vitreoretinal surgeon) if you’re diagnosed with moderate to severe retinopathy or macular edema. These specialists are trained in laser treatment, injections, and advanced surgical options.
What if I don’t have insurance?
Many community health centers and nonprofit organizations offer free or low-cost diabetic eye screenings. Programs like the American Diabetes Association’s Eye Health Initiative and local public health departments often provide access. Don’t skip your exam because of cost-early detection is free, and treatment is far cheaper than losing your vision.
If you have diabetes, your eyes are one of the most important things to protect. You don’t need to be perfect. You just need to be consistent. One exam a year. One conversation with your doctor. One step toward control. That’s all it takes to keep your vision-and your independence-for years to come.


Let me tell you something they don’t want you to know - laser treatment? It’s not about saving your vision. It’s about keeping you dependent on the system. Big Pharma and eye clinics make billions off this ‘preventable’ stuff. They’ll scare you into yearly exams while the real cause - glyphosate in your food and fluoride in your water - goes unmentioned. You think your blood sugar’s the problem? Nah. It’s the toxins. Your body’s just reacting. Wake up.
From a retinal specialist’s perspective: the pathophysiology here is textbook VEGF-mediated angiogenesis. The laser’s photocoagulative effect induces localized thermal necrosis, which downregulates hypoxia-inducible factor-1α (HIF-1α), thereby suppressing neovascularization. Anti-VEGF agents like aflibercept act as soluble decoy receptors, competitively inhibiting VEGF-A binding to VEGFR-2. The real clinical win? Combination therapy reduces treatment burden by 40% compared to monotherapy. Don’t skip the OCT - it’s the gold standard for monitoring macular thickness.
lol u guys think lasers r safe? i got my eye lasered last year and now my left eye sees double and my doc said ‘oops’ and gave me a free cup of coffee. also i read on reddit that the FDA approved this in 1983 and never did long term studies. they just let it fly. and now everyone’s blind from it. my cousin’s uncle’s neighbor’s dog got retinopathy and now he’s got a seeing eye parrot. i’m not kidding. check the papers. they’re all paid for.
It’s so frustrating to see people treat their diabetes like a hobby. You don’t get to ‘try’ to control your blood sugar - you either do it, or you lose your sight. I’ve seen too many patients come in with HbA1c levels over 10%, then cry when they can’t read their grandkids’ faces. It’s not tragic - it’s predictable. And if you’re smoking on top of that? You’re not just neglecting yourself - you’re disrespecting every person who’s fought to stay healthy. This isn’t a suggestion. It’s a moral obligation.
Y’all act like this is some big secret, but it’s obvious - America’s got the best eye care in the world. If you’re still going blind from diabetes, you’re just lazy. Get off the soda, stop eating that cheap rice, and get your A1c checked. I’m a vet - I’ve seen guys come back from Iraq with worse injuries and still drive and read. You wanna keep your vision? Act like it matters. No excuses. America doesn’t reward whiners.
Statistical analysis of the NEI dataset reveals a 68% asymptomatic progression rate, which aligns with the 2018 meta-analysis by Chen et al. (JAMA Ophthalmology). However, the 95% preservation rate post-laser is misleading - it reflects relative risk reduction, not absolute. The baseline risk of severe vision loss is 12%, so absolute risk reduction is only 6.8%. Furthermore, the cost-effectiveness of anti-VEGF therapy is questionable in low-income populations, where treatment adherence drops below 40% due to logistical barriers. The article underestimates systemic inequities.
So let me get this straight - you’re telling me the solution to a disease caused by corporate sugar addiction is to burn holes in your eyes with lasers? Brilliant. Just brilliant. Meanwhile, the same corporations that flood our food with high-fructose corn syrup are funding these ‘preventative’ clinics. They don’t want you cured - they want you compliant. Laser treatment? It’s just a Band-Aid on a bullet wound. And you’re all applauding it like it’s science.
I appreciate the clarity of this post. As someone who works with diabetic patients in underserved communities, I can confirm that the biggest barrier isn’t awareness - it’s access. Many people don’t have transportation to eye clinics, or they’re working two jobs and can’t take time off. We’ve partnered with local pharmacies to offer free screenings on weekends. It’s not glamorous, but it saves sight. Thank you for emphasizing consistency over perfection - that’s the message that actually helps.