When your big toe suddenly swells up, burns like fire, and makes even a bedsheet feel unbearable, you’re not just having a bad night-you’re experiencing a gout flare. This isn’t just "old man pain." Gout affects millions worldwide, and behind the agony is a quiet biochemical storm: purine metabolism gone wrong. Your body breaks down purines-natural compounds in food and your own cells-into uric acid. When too much builds up, it forms sharp crystals in your joints. That’s gout. And fixing it isn’t about cutting out beer alone. It’s about understanding how your body makes uric acid, how to lower it safely, and which medications actually work.
How Purine Metabolism Turns Into Joint Pain
Your body is constantly recycling DNA and RNA from dead cells. That process releases purines. Normally, those purines get broken down step by step into uric acid, then flushed out through your kidneys and gut. But here’s the catch: humans lost the enzyme that turns uric acid into something harmless about 15 million years ago. So we’re stuck with it. And if your body makes too much, or your kidneys can’t flush it out fast enough, uric acid piles up. The tipping point? 6.8 mg/dL. That’s the level where uric acid starts forming crystals. Once that happens, your immune system attacks them like invaders. That’s the redness, heat, and swelling you feel. About 90% of gout cases come from your kidneys not excreting enough uric acid-not from eating too much steak. But diet still matters. Organ meats like liver pack 240-400 mg of purines per 100 grams. Anchovies? 500 mg. Beer? Up to 20 grams per liter. Those numbers aren’t myths-they’re measured facts.Why Most People Don’t Get Better on Gout Meds
Doctors often start patients on allopurinol, a cheap, old drug that blocks the enzyme xanthine oxidase, the last step in uric acid production. It works-but only if you take enough. Studies show 92% of patients hit their target uric acid level when allopurinol is slowly increased to 300 mg or more daily. Yet most people stay on 100 mg. Why? Fear of side effects. But here’s the truth: the risk of serious rash is under 1% if you start low and go slow. The real danger is staying on too low a dose. Febuxostat is the newer alternative. It’s stronger. At 80 mg daily, it hits target levels in nearly 67% of patients, compared to 47% with allopurinol. But it comes with a black box warning. The CARES trial found a higher risk of heart-related death with febuxostat-especially if you already have heart disease. That doesn’t mean avoid it. It means you need to talk to your doctor about your heart health before starting.The Real Cost of Treatment-Not Just Money
Allopurinol costs about $4 a month. Febuxostat? Around $59. Pegloticase? Over $16,000 a month. That’s not a typo. Pegloticase is a biologic that breaks down uric acid into allantoin, a harmless compound. It’s life-changing for people with giant tophi-those visible lumps of uric acid crystals under the skin. One patient on Reddit spent 17 months fighting insurance to get it approved. After nine months, his tophi dissolved. But it’s not for everyone. It requires IV infusions every two weeks. And 26% of people have severe reactions during the infusion. You need steroids and antihistamines just to get it. Even when the meds work, flares don’t stop right away. In fact, they often get worse at first. That’s because as crystals start to dissolve, they trigger inflammation. That’s why guidelines say: start colchicine at the same time as your urate-lowering drug. Take 0.6 mg once or twice daily for at least six months. Most patients skip this. Then they quit the main drug because "it didn’t work." It did. They just didn’t protect themselves during the transition.Who Gets Left Behind?
Only 37% of gout patients in the U.S. ever reach their target uric acid level. Why? Three big reasons: doctors don’t titrate doses, patients stop because of side effects, and no one checks uric acid levels after the first visit. A 2024 study found only 29% of primary care doctors follow the simple rule: test uric acid every 2-5 weeks until the target is hit, then every six months. That’s not just poor care-it’s preventable failure. And it’s not just about access. Genetic factors matter. Some people carry a variant of the SLC2A9 gene that makes their kidneys reabsorb more uric acid. Others have HLA-B*58:01, which puts them at high risk of a dangerous skin reaction to allopurinol. Testing for this gene isn’t routine yet-but in places like New Zealand and parts of Asia, it’s becoming standard before starting allopurinol. If you’re of Māori, Pacific Islander, or East Asian descent, ask your doctor if testing is right for you.What’s Coming Next?
The future of gout treatment is getting smarter. Verinurad, a new drug that blocks uric acid reabsorption in the kidneys, is in late-stage trials. When paired with febuxostat, it helped 74% of patients reach target levels in just 12 weeks. Arhalofenate, another new drug, doesn’t just lower uric acid-it also reduces inflammation, cutting flare frequency by more than half. These aren’t just lab results. They’re real hope for people tired of living in fear of the next flare. The big shift? Moving from "take a pill and hope" to personalized treatment. We’re starting to use genetics, kidney function, and even gut microbiome data to choose the right drug for the right person. No more trial and error. No more guessing.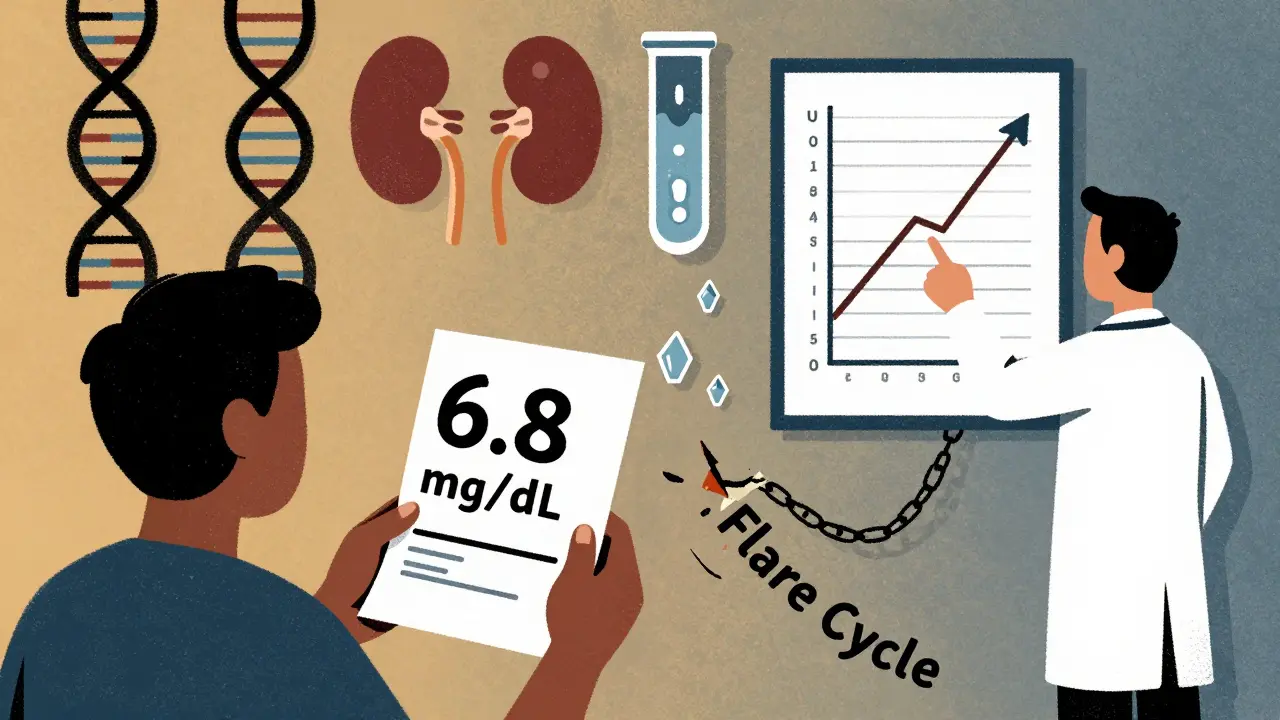
What You Can Do Today
If you have gout, here’s what matters most:- Ask for your serum uric acid level. Know the number.
- If you’re on allopurinol, ask if your dose can be increased. Most people need 300 mg or more.
- Start colchicine at the same time as your urate-lowering drug. Don’t wait.
- Get your kidney function checked. If your eGFR is below 30, febuxostat may be safer than allopurinol.
- Limit organ meats, shellfish, and beer. But don’t blame your diet for your gout-it’s rarely the main cause.
- Track your flares. If you’re having more than one a year, your treatment isn’t working.
Frequently Asked Questions
Can I stop taking urate-lowering meds if my gout feels better?
No. Gout is a chronic condition caused by high uric acid levels. Stopping medication lets uric acid rise again, and crystals will reform. Even if you haven’t had a flare in years, stopping your drug puts you at high risk of returning pain and permanent joint damage. Lifelong treatment is the standard for most patients.
Is allopurinol safe if I have kidney disease?
Yes, but you need a lower starting dose and slower increases. For people with moderate kidney disease (eGFR 30-59), doctors start at 50 mg daily and increase slowly. If your kidney function is severely reduced (eGFR below 30), febuxostat is often preferred because it’s cleared by the liver, not the kidneys. Always get your kidney function tested before starting or changing treatment.
Why do I get flares when I start taking allopurinol?
As uric acid levels drop, existing crystals begin to dissolve. This releases particles that trigger inflammation-like stirring up sediment in a bottle. It’s not the drug causing the flare; it’s your body cleaning up. That’s why doctors prescribe colchicine or low-dose NSAIDs during the first 6 months. This prevents flares while your body adjusts.
Can diet alone cure gout?
No. Even a strict low-purine diet typically lowers uric acid by only 1-2 mg/dL. That’s not enough for most people. Diet helps, but it’s an add-on, not a replacement for medication. If you think you can "eat your way out" of gout, you’re setting yourself up for repeated flares and long-term joint damage.
What’s the difference between allopurinol and febuxostat?
Both block xanthine oxidase, the enzyme that makes uric acid. Allopurinol is older, cheaper, and works well for most people if dosed correctly. Febuxostat is stronger and doesn’t need kidney adjustment, but it carries a higher risk of heart-related death in people with existing heart disease. Allopurinol is still first-line for most. Febuxostat is for those who can’t tolerate allopurinol or have severe kidney issues.
Is pegloticase worth the cost?
For people with severe tophaceous gout-where crystals have formed large, painful lumps under the skin-yes. It’s the only treatment that can dissolve those tophi. But it’s not for mild or moderate gout. It’s expensive, requires IV infusions, and has serious risks. It’s reserved for patients who’ve tried and failed at least two other drugs. Insurance often requires proof of failure before approving it.


The article nails the biochemistry but misses the clinical reality: most patients are never titrated properly. Allopurinol at 100 mg is a placebo dose. Xanthine oxidase inhibition requires saturation, and if your doc isn't pushing to 300-600 mg, they're not treating gout-they're just appeasing the patient. The 92% success rate with adequate dosing isn't controversial-it's evidence-based dogma. Stop underdosing. Stop blaming diet. Stop pretending this is a lifestyle issue. It's a metabolic disorder with a pharmacologic solution, and we're failing patients systematically.
I appreciate how this breaks down the science without jargon overload. I had gout for years and thought it was just beer and steak. Turns out my kidneys were the issue. I started on allopurinol at 100 mg and felt nothing. When my rheumatologist bumped me to 300 mg and added colchicine, my flares stopped cold. The key is patience. It takes months for crystals to dissolve. Don't quit because your toe hurts more at first. That's the medicine working, not breaking.
So we're told to take drugs because we're broken by evolution. We lost the enzyme 15 million years ago. What does that mean for human purpose. Are we just flawed machines trying to fix biological accidents with pills. The real tragedy isn't gout. It's that we've accepted medicine as a substitute for understanding. We don't ask why we're stuck with uric acid. We just take the pill. And that's the real disease. Complacency disguised as treatment.
As someone with a South Asian background, I'm glad the article mentioned HLA-B*58:01. My uncle had a severe reaction to allopurinol-hospitalized for SJS. We didn't know about genetic testing until it was too late. Now I make sure every family member gets screened before any purine-lowering meds. It's not just about cost or access. It's about cultural awareness in medicine. If you're from the Indian subcontinent, Africa, or East Asia, ask for the test. It could save your life.
Oh sweet Jesus another doctor blog pretending they're the first to discover that diet doesn't cure gout. Congrats. You've read a textbook. Meanwhile, my cousin in Nigeria is drinking palm wine and eating smoked fish daily and hasn't had a flare in 12 years. Maybe the real issue isn't purines. Maybe it's that Western medicine is obsessed with pills because pills make money. Just saying.
For anyone reading this and thinking "I'll just change my diet"-please don't. I did. Lost 30 lbs, cut out beer, went vegan. My uric acid dropped from 9.2 to 7.8. Still had flares every 3 months. Started allopurinol at 300 mg + colchicine. Zero flares in 18 months. Diet helps. But it's not the cure. Medication is. And colchicine isn't optional-it's the bridge. If your doctor didn't tell you that, find a new one.
Western medicine always thinks they know better. In Nigeria we use ginger, garlic, and bitter leaf juice. My father had gout for 40 years. He never took a pill. He walked every morning. He drank herbal tea. He lived to 89. You think a lab test and a $59 pill is better than ancestral wisdom. You're wrong. This article is just another colonial scam to sell drugs to poor people who dont know better.
Allopurinol works but only if you dont stop it after 3 months. Most patients quit because of the first flare. They think its the drug. Its the crystals dissolving. The article says it. No one listens. Thats why 63% fail. Its not the meds. Its the mindset. Fix that first.