Getting your medications right isn’t just about picking up prescriptions. It’s about knowing when to take them, why you’re taking them, and what to do if something goes wrong. Too many people end up confused, skipping doses, or doubling up because no one took the time to walk them through it. A Medication Action Plan (MAP) changes that. It’s not just a list of pills. It’s your personalized roadmap to staying safe and healthy with your meds.
What Exactly Is a Medication Action Plan?
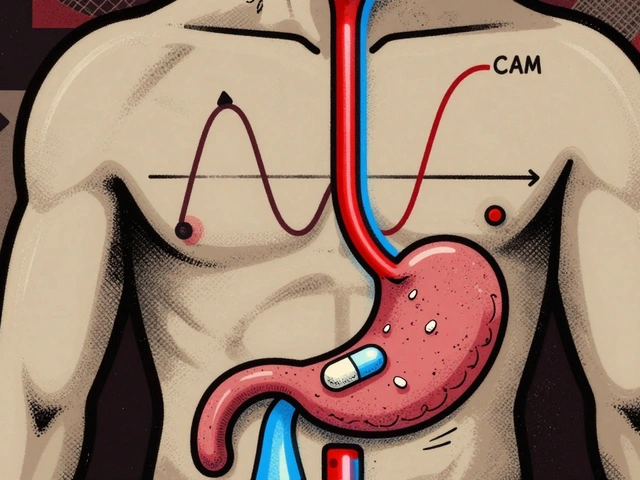
A Medication Action Plan is a written, step-by-step guide you create with your care team-your doctor, pharmacist, or nurse-to help you take your medicines correctly. Unlike a simple prescription list, it includes actions you can actually do. For example: "Take your blood pressure pill after brushing your teeth every morning" or "If you feel dizzy after taking your diabetes medicine, sit down and check your blood sugar. Call your doctor if it’s below 4.0 mmol/L." It’s built around your life, not the other way around. If you forget pills because you’re always rushing out the door, your plan might include putting your pill organizer next to your keys. If you take five different meds for different conditions, your plan might use color-coded sections: blue for heart meds, green for diabetes, red for pain. This isn’t theoretical. In Germany, since 2016, patients taking three or more prescription drugs get a standardized medication plan from their pharmacist. Studies show this cuts medication errors by up to 40%.Why Your Care Team Needs to Be Involved
You can’t build this alone. Your doctor knows what you’re being treated for. Your pharmacist knows how the drugs interact. You know your schedule, your habits, your fears. The best plans come from all three working together. For example, your doctor might prescribe a new cholesterol drug. But your pharmacist notices you’re also taking a common over-the-counter painkiller that can raise your blood pressure. Together, you adjust your plan: swap the painkiller, add a daily walk, and set a reminder to check your BP twice a week. Without that conversation, you might never know the two were clashing. And it’s not just about prescriptions. Vitamins, herbal supplements, even antacids can interfere. A 2021 survey of Medicare patients found that 68% didn’t tell their doctor about the supplements they were taking. That’s a gap a Medication Action Plan closes.Step-by-Step: How to Create Your Plan
Step 1: Gather everything you take Before your meeting, collect every pill, capsule, patch, or liquid you use. That includes:- Prescription drugs
- Over-the-counter meds (like ibuprofen or sleep aids)
- Vitamins and minerals
- Herbal supplements (ginseng, turmeric, St. John’s wort)
- Topical creams or eye drops
- "I take my morning pill after coffee, but sometimes I skip it if I’m late."
- "I don’t know why I’m taking this one-it was just handed to me."
- "I get nauseous after my pain meds, so I stop taking them."
- "Take your blood pressure pill at 7 a.m., right after you brush your teeth."
- "If you miss a dose, take it within 8 hours. If it’s later, skip it. Don’t double up."
- "Check your BP twice a week and write it down in the notebook next to your pill organizer."
What Makes a Plan Work-or Fail
Not all plans are created equal. Here’s what works:- Specific actions: "Take pill after breakfast" > "Take pill daily."
- Measurable goals: "Take 9 out of 10 doses this week" > "Try to take your meds."
- Clear triggers: "If your knee swells, call the clinic before taking more naproxen."
- Personal fit: If you’re a night owl, don’t schedule morning doses.
- Generic templates with no personalization
- Plans full of terms like "hypertension" or "polypharmacy"
- Plans that don’t include OTC meds or supplements
- Plans that sit in a drawer and never get updated
How Often Should You Update It?
Your plan isn’t set in stone. Change happens:- When you start or stop a medicine
- When you get a new diagnosis
- When you change your routine (retirement, travel, moving)
- When you notice side effects

What If Your Care Team Doesn’t Offer This?
You’re not stuck. Here’s what to do:- Ask your pharmacist: "Can we do a medication review?" Most pharmacies offer this for free.
- Call your insurance. Ask: "Do I qualify for Medication Therapy Management?" Even if you’re not on Medicare, many private plans now cover it.
- Use free tools. The CDC and American Pharmacists Association have printable MAP templates online.
- Bring a family member. Two heads are better than one when remembering details.
Real Results: Why This Matters
This isn’t just about remembering pills. It’s about staying out of the hospital. In the U.S., medication errors lead to 280,000 hospital stays every year. For people on multiple drugs-like those with diabetes, heart disease, and arthritis-the risk is even higher. But studies show that patients who use personalized Medication Action Plans:- Improve adherence by 25-40%
- Have 32% fewer medication-related hospital visits in the next year
- Report feeling more in control of their health
Final Thought: Your Health, Your Plan
You’re not just a patient. You’re the most important person in your care team. No one knows your body, your schedule, your fears better than you. A Medication Action Plan puts you in charge-not with pressure, but with clarity. It turns confusion into confidence. It turns forgetfulness into routine. And it turns a pile of pills into a path to feeling better.Start today. Gather your meds. Call your pharmacist. Ask for a plan. You’ve earned it.
What’s the difference between a medication list and a Medication Action Plan?
A medication list just shows what drugs you take-names, doses, times. A Medication Action Plan goes further. It tells you what to do when things go wrong, how to fit pills into your daily life, and what signs mean you need help. It’s action-oriented, personalized, and designed for real-life use-not just record-keeping.
Can I make a Medication Action Plan on my own?
You can start one, but it won’t be as safe or complete. Without input from your pharmacist or doctor, you might miss drug interactions, incorrect doses, or duplicate medications. A plan created with your care team uses expert knowledge and your personal context together. That’s what makes it effective.
Do I need to be on Medicare to get a Medication Action Plan?
No. While Medicare Part D requires plans to offer Medication Therapy Management to eligible members, many private insurers and employer health plans now offer similar services. Pharmacies also often provide free medication reviews regardless of insurance. Ask your pharmacist-they’re trained to help.
What if I don’t understand the medical terms on my plan?
Say so. Right away. A good Medication Action Plan uses plain language. If you see words like "hypertension," "diuretic," or "anticoagulant," ask your pharmacist to rewrite them as "blood pressure pill," "water pill," or "blood thinner." Your plan should make sense to you-not just to a doctor.
How do I know if my plan is working?
Track your adherence for a week. Did you take your pills as scheduled? Did you notice fewer side effects? Did you feel more confident? If you’re taking 90% of your doses and feeling better, your plan is working. If not, go back to your care team. Adjustments are normal-and necessary.
Can my Medication Action Plan be digital?
Yes. Many pharmacies now offer apps that sync with your plan and send reminders. Some even let you upload photos of your pill bottles to auto-fill your list. But digital doesn’t mean automatic. You still need to review and update it regularly. The best plan is the one you’ll actually use-whether it’s on paper, on your phone, or taped to your fridge.


This is the kind of post that actually makes me feel like my health matters. I used to just dump all my pills in a box and hope for the best. Now I’ve got mine taped to my fridge with doodles of coffee cups and bedtimes. Game changer.
Let’s be real-this plan sounds great on paper but ignores systemic healthcare failures. If your pharmacist is overworked and your doctor runs 45 minutes late, who’s really supposed to sit down for a 60-minute review? This is virtue signaling disguised as patient empowerment.
You think this is about health? No. This is corporate medicine’s latest trick to shift blame onto the patient. In India, we don’t need color-coded pill boxes-we need affordable drugs and doctors who aren’t paid by Big Pharma. This ‘plan’ is just another way to make you feel guilty for not being perfect while the real problem-the cost, the greed, the profit-driven system-stays untouched. They want you to fix yourself so they don’t have to fix the system.
I’m from Kenya and I’ve seen how this works in rural clinics-no fancy apps, no pill organizers, just a grandmother with a notebook and a voice that says, ‘Take this after the sun moves past the tree.’ That’s the real MAP. Simple, human, rooted in daily life. This post nails it. No jargon, no fluff. Just ‘do this, watch for that.’ We need more of this everywhere.
Why do we even need a plan? Just take your damn pills. I’m tired of overcomplicating everything. Also, who has time to draw pictures of coffee cups? 😒
I used to think my meds were just a chore until I realized they were the only thing keeping me from becoming a ghost in my own life. The plan didn’t fix me-it gave me back my mornings. No fancy words needed. Just ‘take it after brushing’ and ‘call if you feel like you’re sinking.’ That’s all. And yeah, I cried reading this. Not because it’s sweet. Because it’s true.
My mom’s on 8 meds. She doesn’t read. Doesn’t use apps. So we printed her plan on a big card, laminated it, and hung it by the coffee maker. She points to it now when she’s confused. No one’s perfect. But this? This works. Thanks for writing this.
As a pharmacist in Dublin, I’ve seen this work-and fail. The difference? The person who actually listens. Not the one who rushes through the checklist. If you’re not asking ‘What’s stopping you?’ instead of ‘Did you take it?’ you’re not building a plan-you’re writing a to-do list. And that’s why 68% of patients hide their supplements. They’ve been shamed into silence. This post? It doesn’t shame. It invites. That’s rare.
It’s imperative to acknowledge that the efficacy of a Medication Action Plan is contingent upon a confluence of interdependent variables-namely, patient literacy, pharmacokinetic compatibility, temporal adherence metrics, and the presence of a multidisciplinary care ecosystem. Without a standardized digital interface integrated with EHRs and real-time pharmacovigilance feeds, even the most personalized MAP remains a static artifact, susceptible to cognitive overload, temporal misalignment, and polypharmacy-induced metabolic drift. The absence of automated dose titration protocols and AI-driven adverse event prediction modules renders the entire paradigm vulnerable to human fallibility. We must evolve beyond paper charts and coffee-cup reminders toward closed-loop, biometrically-informed therapeutic orchestration systems that dynamically adapt to physiological feedback. Otherwise, we’re just rearranging deck chairs on the Titanic.