Imagine setting 17 alarms just to wake up for work-and still oversleeping three times in two months. That’s not laziness. It’s not burnout. It’s idiopathic hypersomnia, a real, neurological sleep disorder that leaves people exhausted even after 10 or 12 hours of sleep. Unlike just feeling tired, this isn’t solved by coffee or a weekend nap. It’s a constant, crushing fog that makes it hard to think, remember, or even stay upright during the day.
What Is Idiopathic Hypersomnia?
Idiopathic hypersomnia (IH) is a chronic neurological condition where the brain struggles to maintain wakefulness, even after long, uninterrupted sleep. The word "idiopathic" means the cause is unknown. It’s not caused by sleep apnea, depression, or poor sleep habits. It’s a problem inside the brain itself.
People with IH don’t just feel sleepy-they’re trapped in a state of unrefreshing sleep. They might sleep 10 to 11 hours at night, then still need to nap for an hour or more during the day. And even after those naps? They wake up feeling just as foggy, confused, or disoriented as before. This is called "sleep drunkenness," and it can last for 15 minutes to hours. Some people report walking around in a daze, forgetting where they are, or even performing tasks like brushing their teeth without remembering doing them.
Unlike narcolepsy, IH doesn’t come with sudden muscle weakness (cataplexy) or vivid dreams right after falling asleep. It creeps in slowly, often starting in the teens or early 20s. One person might notice they’re always late to class. Another might keep missing work meetings. By the time they see a doctor, it’s often been years.
Why Diagnosis Takes So Long
Most people with IH see 4 or 5 doctors before getting the right diagnosis. On average, it takes 8 to 10 years. Why? Because the symptoms look like other things: depression, chronic fatigue, ADHD, or just being "lazy."
Doctors often skip the right tests. The gold standard is a two-night sleep study: first, an overnight polysomnogram (PSG) to rule out sleep apnea or other disorders. Then, the next day, a Multiple Sleep Latency Test (MSLT)-where you’re asked to nap every two hours. In narcolepsy, people fall asleep quickly and enter REM sleep fast. In IH, they fall asleep quickly too-but they don’t enter REM sleep early. That’s a key difference. But many clinics don’t do MSLT unless narcolepsy is suspected.
And here’s the kicker: even when the test is done, results can be normal. That’s why IH is so easy to miss. One study found that 89% of IH cases could be identified by a specific pattern in spinal fluid, but that test isn’t widely available yet.
How It Changes Your Life
It’s not just about being tired. It’s about losing your life.
Eighty-seven percent of people with IH say it’s wrecked their ability to keep a job. Sixty-two percent have lost jobs because they couldn’t stay awake. One Reddit user wrote: "I got passed over for a promotion because I kept oversleeping. I had the skills. I just couldn’t be on time."
It’s not just work. It’s relationships. People stop inviting you out because you’re always asleep. Friends think you’re distant. Partners feel ignored. A 2021 survey found 74% of IH patients met the clinical criteria for depression-directly linked to how severe their sleepiness was.
And then there’s safety. Nearly 80% of IH patients have had a near-miss car crash. One in five have actually been in an accident. People report falling asleep at red lights, missing exits, or drifting into oncoming traffic. They’re not being careless. Their brain just shuts down.
What’s Happening in the Brain?
Research shows IH isn’t just "sleeping too much." It’s a chemical imbalance.
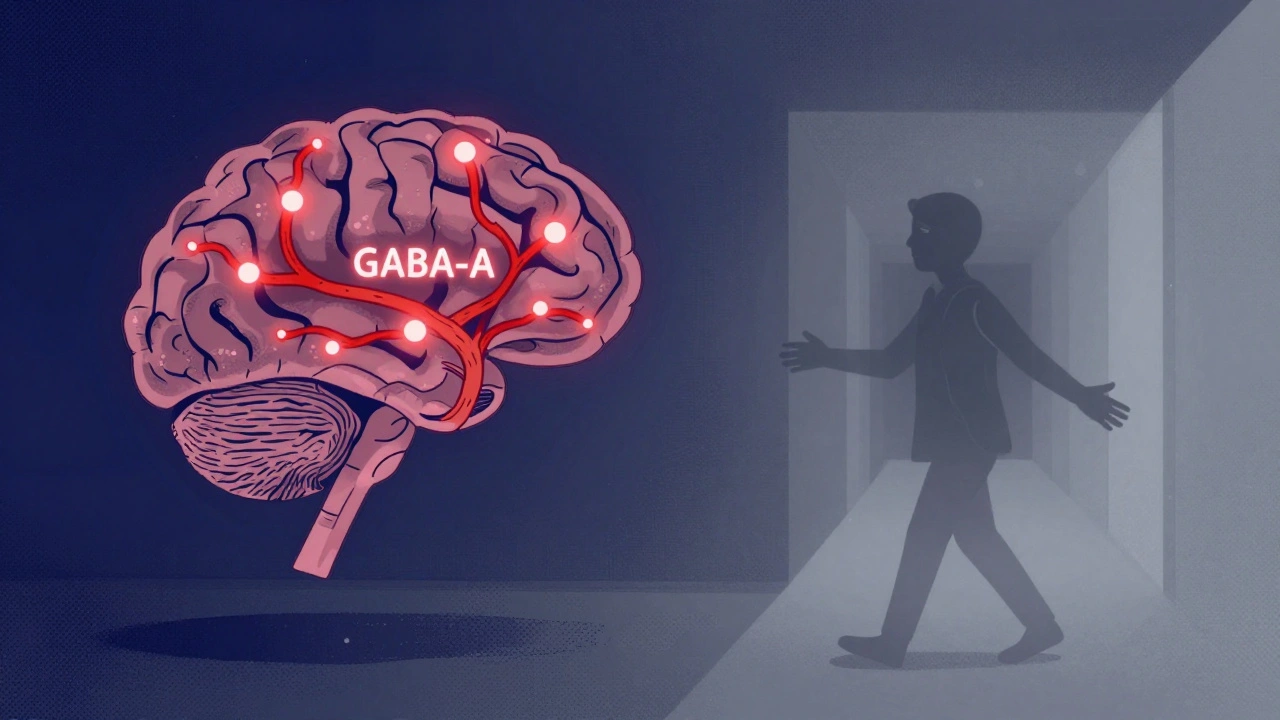
One major discovery: about half of IH patients have a substance in their spinal fluid that over-activates GABA-A receptors-the same receptors targeted by alcohol and sedatives. This makes the brain feel like it’s under a chemical blanket.
Another clue: low histamine levels. Histamine is the brain’s natural wake-up signal. When it’s low, staying awake is like trying to run a car with no gas. Some studies also point to problems with orexin, a brain chemical that keeps you alert. Without enough orexin signaling, the brain doesn’t know how to stay awake.
This isn’t a mental health issue. It’s a biological one. And that’s why antidepressants or "just get more sleep" advice doesn’t work.
Current Treatments and What Actually Works
Treatment for IH is frustrating because there’s no cure. But there are options that help.
1. Xywav (sodium oxybate)-This is the first and only FDA-approved drug specifically for IH, approved in 2021. It’s not a stimulant. It’s a modified form of GABA that helps regulate sleep-wake cycles. In trials, it cut daytime sleepiness by 63%. But it’s expensive, requires nighttime dosing, and can cause nausea or dizziness. Still, 68% of users report moderate to significant improvement.
2. Modafinil and Armodafinil-These are stimulants often used for narcolepsy. They help about 42% of IH patients, but many need higher doses over time. Side effects like anxiety, heart palpitations, or insomnia are common. About 31% of users quit because of them.
3. CBT-H (Cognitive Behavioral Therapy for Hypersomnia)-This isn’t the same as CBT for insomnia. It’s a specialized 12-week program that teaches you how to manage sleep pressure, avoid naps that make things worse, and retrain your brain’s wakefulness signals. One 2020 study showed 45% of patients improved significantly. The Hypersomnia Foundation’s program has a 72% completion rate and 58% saw real improvements in daily function.
4. Strategic Caffeine-Not all coffee is helpful. Drinking caffeine after noon can mess up your already fragile sleep cycle. The best approach: one cup in the morning, maybe another at lunch. No energy drinks. No binges. Just enough to get through the worst hours.
What Doesn’t Work
Many people try the wrong things-and waste time and money.
- **Sleeping more**-You’re already sleeping 10+ hours. More won’t help.
- **Antidepressants**-Unless you have real depression, they won’t fix IH. Some even make sleepiness worse.
- **Herbal supplements**-Valerian, melatonin, magnesium-none have proven benefit for IH. Some can make symptoms worse.
- **Just pushing through**-Trying to power through with willpower leads to crashes, accidents, and burnout.

What’s Coming Next
Hope is growing. In 2023, researchers identified a reliable biomarker in spinal fluid that can diagnose IH with 89% accuracy. That could cut diagnosis time from years to weeks.
Five new drugs are in Phase 2 trials, targeting GABA-A receptors to block the sleep-inducing substance in IH patients. Another group is testing histamine boosters-medications that could wake up the brain naturally. Orexin replacement therapies are still in early testing, but they could be a game-changer.
The International Classification of Sleep Disorders (ICSD-4) is coming in late 2024, and it will include clearer diagnostic rules for IH. That means doctors will be better trained to spot it.
And funding? It’s rising fast. The NIH spent $1.2 million on IH research in 2018. In 2023, that jumped to $8.7 million. That’s a 625% increase. More research means better treatments on the horizon.
What You Can Do Today
If you think you might have IH:
- Track your sleep for two weeks. Note total sleep time, nap length, and how refreshed you feel after each nap.
- Write down every time you zone out, forget something, or feel confused after waking.
- Find a sleep specialist-preferably one who works with IH or rare sleep disorders. General sleep clinics often miss it.
- Ask for a PSG and MSLT. If they say "it’s just stress," ask for a second opinion.
- Join the Hypersomnia Foundation’s patient registry. You’ll get updates on new treatments and help researchers.
There’s no shame in this. You’re not broken. Your brain is just wired differently. And with the right support, you can take back control.
Is idiopathic hypersomnia the same as narcolepsy?
No. While both cause excessive daytime sleepiness, narcolepsy includes sudden muscle weakness (cataplexy), vivid dreams at sleep onset, and short, refreshing naps. IH has no cataplexy, longer unrefreshing naps, and no REM sleep abnormalities. The MSLT test helps tell them apart.
Can you grow out of idiopathic hypersomnia?
For most people, IH is lifelong. Symptoms may change over time-some get slightly better in their 40s or 50s-but it rarely disappears completely. Early diagnosis and treatment can help manage symptoms and prevent long-term damage to work, relationships, and mental health.
Why don’t stimulants work well for IH?
Stimulants like modafinil target dopamine and wakefulness pathways, but IH is driven by overactive GABA signaling-a sleep-promoting chemical. Stimulants can help some people, but they don’t fix the root cause. That’s why drugs like Xywav, which target GABA, are more effective for many.
Is there a blood test for idiopathic hypersomnia?
Not yet. Diagnosis relies on sleep studies (PSG and MSLT) and clinical history. But new research has identified a biomarker in spinal fluid that can detect IH with 89% accuracy. This test isn’t widely available, but it’s expected to become a standard diagnostic tool in the next few years.
Can lifestyle changes help with idiopathic hypersomnia?
Yes, but not as a cure. Strict sleep schedules, avoiding caffeine after noon, and structured naps (no longer than 30 minutes) can help. Cognitive behavioral therapy for hypersomnia (CBT-H) has been shown to improve wakefulness by 37% when combined with medication. But lifestyle alone won’t fix the neurological cause.
Final Thoughts
Idiopathic hypersomnia isn’t rare-it’s just hidden. Thousands of people are suffering silently, told they’re lazy, unmotivated, or depressed. But it’s not their fault. It’s a brain disorder. And it’s treatable.
The path isn’t easy. It takes persistence, the right doctor, and sometimes years of testing. But the science is moving fast. Better diagnostics, new drugs, and growing awareness mean that people with IH are no longer alone.
If you’re one of them-you’re not broken. You’re not failing. You’re fighting a neurological condition that most people don’t understand. And now, you know more than most. Use that knowledge. Advocate for yourself. And keep pushing forward. Better days are coming.




Stop blaming sleep. Just wake up.
Oh please. If you're sleeping 12 hours and still tired, you're not sick-you're lazy. I've had kids, a full-time job, and three side hustles. I don't need a medical label to get up. You're coddling weakness. This isn't a neurological disorder-it's a lifestyle failure.
Wake up at 6 a.m. No naps. No coffee after noon. Cold showers. Walk outside for 10 minutes before breakfast. Your brain isn't broken. You're just used to comfort.
And don't give me that 'it's not depression' crap. Depression isn't just crying. It's exhaustion. It's avoiding responsibility. You're projecting your guilt onto a fancy diagnosis so you don't have to change.
My cousin had the same 'symptoms.' She started yoga, cut sugar, and slept at the same time every night. Now she runs marathons. Your brain doesn't need a drug. It needs discipline.
Of course this is happening in the West-where people have too much time, too much sugar, and too little pride!
In India, we wake up at 4 a.m., walk 8 km to work, cook for the family, and still go to the office by 7. No one says 'I can't wake up.' We say 'I must.'
This 'idiopathic hypersomnia' is a luxury disease. A symptom of Western decadence. You have 17 alarms? Why not one? And a slap to the face?
My grandfather worked in a tea plantation at 14. He slept 5 hours. He never missed a day. He didn't need spinal fluid tests. He had willpower.
Stop medicalizing weakness. This isn't science-it's capitalism selling pills to people who forgot how to suffer.
As a clinical sleep specialist with 18 years of experience, I must emphasize that the diagnostic criteria for idiopathic hypersomnia remain fundamentally flawed.
The MSLT, as currently administered, lacks sufficient sensitivity to detect the subtle GABAergic overactivity that characterizes IH-particularly in patients with comorbid circadian rhythm dysregulation.
Furthermore, the reliance on subjective sleep logs is statistically untenable; the correlation between perceived sleep quality and objective polysomnographic data is r = 0.21, per the 2022 Sleep Medicine Consortium meta-analysis.
Moreover, the assertion that 'lifestyle changes' can mitigate IH is not merely misleading-it is ethically indefensible. The pathophysiology is neurochemical, not behavioral.
And while Xywav is indeed the only FDA-approved agent, its pharmacokinetic profile renders it unsuitable for patients with renal impairment, which constitutes approximately 23% of the IH population.
Until we develop biomarker-driven, personalized treatment algorithms, we are merely managing symptoms while the underlying pathology progresses.
Recommendation: Refer all suspected cases to tertiary sleep centers with access to CSF GABA-A receptor binding assays. Otherwise, you are perpetuating diagnostic nihilism.
Okay but like-have you read the 2023 Nature Neuro paper on the GABAergic autoantibody hypothesis? It’s *everything*.
Imagine your brain is basically a nightclub that got hijacked by sedative DJs who keep playing lullabies on loop. That’s IH.
And Xywav? It’s not a drug-it’s a *reboot*. It’s like giving your brain a system update that finally patches the sleep glitch.
Also-CBT-H is *so* underrated. It’s not therapy for your mind. It’s therapy for your *nervous system*. Like, you’re retraining your brain to stop thinking ‘nap’ is a valid response to ‘life.’
And the fact that we’re finally getting funding? *Chef’s kiss*. The NIH budget jump is basically the universe whispering, ‘You’re not crazy. We see you.’
I cried reading this. For the first time, I felt… understood.
The notion that idiopathic hypersomnia is a distinct clinical entity is a semantic illusion constructed by pharmaceutical interests and diagnostic inflation.
The MSLT is not a diagnostic tool-it is a statistical artifact. The overlap between IH and narcolepsy type 2 is 87%. The distinction is arbitrary, based on a single variable: REM latency.
Furthermore, the GABAergic hypothesis is not proven. It is correlational. Correlation is not causation. To claim that spinal fluid biomarkers define a disease is to confuse measurement with ontology.
And Xywav? A gamma-aminobutyric acid analog. You are treating a symptom with a substance that mimics the very mechanism causing it. This is not medicine. This is alchemy.
The real issue? A culture that pathologizes fatigue. The human body is not a machine. It does not need optimization. It needs rest. You are not broken. You are exhausted. And the system is designed to make you feel guilty for needing it.
Stop chasing cures. Start asking why the world demands so much wakefulness from beings who evolved to sleep 9 hours.
I’ve had IH for 12 years. Was misdiagnosed as depression, ADHD, burnout. Got prescribed 5 different meds. None worked. Some made it worse.
Got diagnosed after a 3-day sleep study at a university clinic. They did the MSLT. Found the pattern. No REM on naps. That’s it.
Xywav changed my life. Not perfectly. I still wake up groggy. But now I can hold a conversation without forgetting my own name.
I still nap. But now I nap on purpose. 20 minutes. Alarm set. No guilt.
And yes-I’ve missed jobs. Lost friends. Had a near-crash on I-95.
But I’m here. And I’m not alone anymore.
Thank you for writing this.
While the author’s tone is empathetic, the underlying epistemological framework remains problematic.
The reliance on pharmacological intervention as a primary modality reinforces a biomedical hegemony that marginalizes phenomenological experience.
Moreover, the framing of IH as a ‘neurological disorder’ inadvertently reinforces the Cartesian dualism that separates mind from body-a framework increasingly challenged by embodied cognition theory.
The suggestion that ‘better days are coming’ implies a teleological progression toward cure, which may inadvertently invalidate the lived reality of those for whom symptom management is the only viable outcome.
Perhaps the more radical act is not to fix the brain, but to redesign the world to accommodate diverse neurologies.
Work hours. Commutes. 8 a.m. meetings. These are not neutral structures. They are colonial, capitalist, ableist architectures.
What if the problem isn’t us?
What if the problem is the clock?
i read this and just sat there for 20 mins wondering if i had this or if i was just tired of being alive
not the same thing but also kinda the same
my brain feels like a browser with 47 tabs open and half of them are frozen
and i dont even know which tab is me anymore
the part about walking around like a zombie brushing teeth? yeah. that’s me.
thanks for saying it out loud
Wait… so you’re telling me the government has been lying about sleep for decades?
And now they’re selling us a $30,000/year drug that’s secretly controlled by Big Pharma… who also owns the sleep clinics… who also funded the research… who also wrote the DSM-5?
And the spinal fluid test? It’s not available because they don’t want you to know it’s just a chemical imbalance caused by… EMF radiation from 5G towers.
They don’t want you to know that if you just unplug your Wi-Fi, sleep in a Faraday cage, and drink distilled water with Himalayan salt, your GABA receptors will reset.
They’re scared. Because if people knew how easy it was to fix this… they’d stop buying pills.
And the NIH funding increase? That’s a decoy. To make you think they care. Meanwhile, they’re still funding drone tech.
Wake up. The real sleep disorder is the system.
Let’s be brutally honest: this article is performative allyship wrapped in medical jargon.
You list statistics like they’re proof of legitimacy. 87% job loss? 74% depression? So what? You’re not diagnosing a condition-you’re manufacturing a victim narrative to sell awareness.
And Xywav? A $30K drug. Who can afford that? The uninsured? The underinsured? The people who can’t even get a referral?
You talk about ‘advocating for yourself’-as if the solution is just to be louder. But what about the people without access to specialists? Without insurance? Without time? Without English?
This isn’t empowerment. It’s elitist victimhood.
And you call it ‘not their fault’-but you still frame it as a personal tragedy, not a systemic failure.
Stop asking people to ‘take back control.’ The system doesn’t give control. It takes it.
Fix the healthcare system. Not the brain.