When someone suddenly struggles to breathe, their skin breaks out in hives, and their throat feels like it’s closing - this isn’t just a bad allergy. It’s anaphylaxis, a life-threatening reaction that can kill in minutes if not treated right away. There’s no waiting. No hoping it gets better. And no substitute for epinephrine.
What Exactly Is Anaphylaxis?
Anaphylaxis isn’t a rash or a stuffy nose. It’s a full-body emergency triggered by your immune system going into overdrive. It usually starts within minutes after exposure to something you’re allergic to - like peanuts, shellfish, a bee sting, or penicillin. In 80-90% of cases, you’ll see skin symptoms: hives, swelling of the lips or eyelids, or flushing. But here’s the catch: if you only see skin symptoms, you’re not safe. The real danger is what comes next - trouble breathing, a drop in blood pressure, or vomiting and diarrhea.
The official diagnosis requires one of two things: either skin symptoms plus breathing or circulation problems, or two or more of these: skin issues, breathing trouble, low blood pressure, or gut symptoms - all happening fast after exposure to a likely trigger. This isn’t guesswork. It’s a medical emergency that demands immediate action.
Why Epinephrine Is the Only Treatment That Saves Lives
Antihistamines like Benadryl? They help with itching or a runny nose - but they do nothing to stop anaphylaxis. Steroids? They might help prevent a second wave of symptoms hours later, but they won’t save you now. Only epinephrine works fast enough to reverse the life-threatening effects.
Epinephrine works in two ways: it tightens blood vessels to raise blood pressure and opens up airways so you can breathe. In a study of over 1,200 anaphylaxis cases, 97% of emergency doctors said epinephrine was the only treatment that mattered. Patients who got it within 5 minutes were 85% more likely to improve than those who waited. Delaying it is the single biggest reason people die from anaphylaxis.
There’s no other drug that does this. No pill. No spray. Not even the new nasal epinephrine (Neffy) - which is helpful - can replace the speed and reliability of the auto-injector in most situations. Epinephrine is the only treatment proven to prevent death.
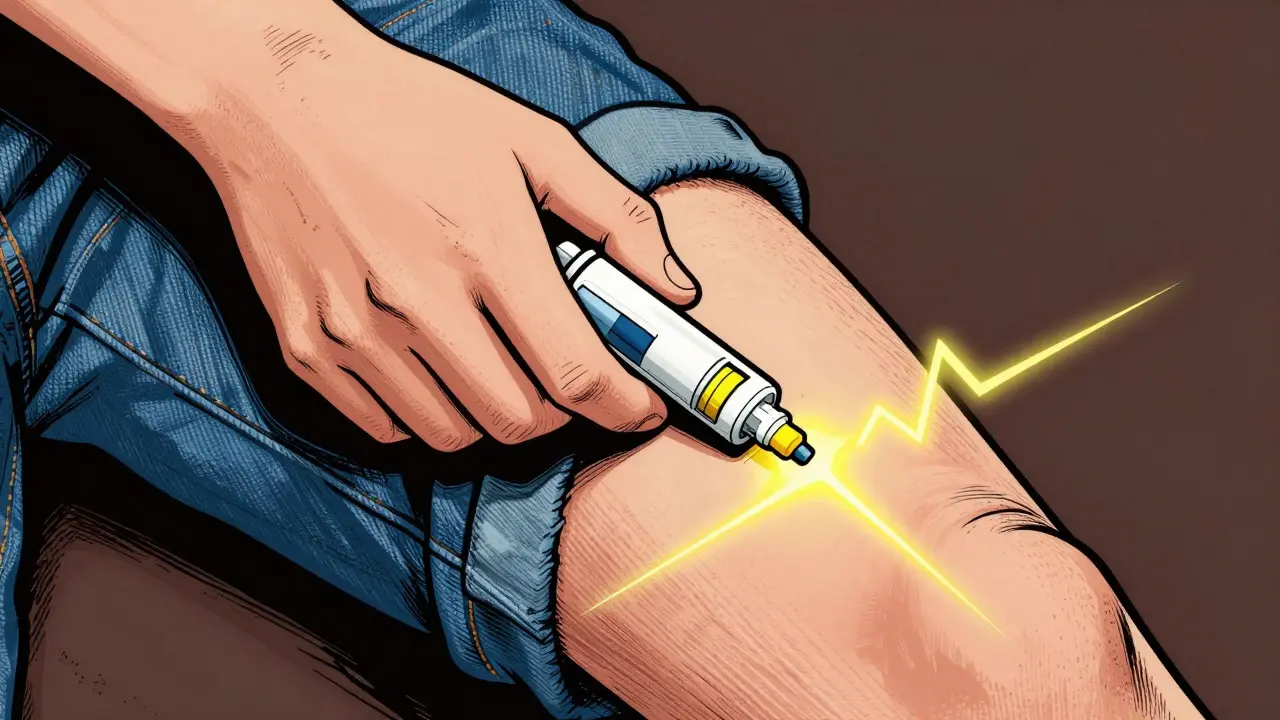
How to Use an Epinephrine Auto-Injector
You don’t need to be a doctor to use one. But you do need to practice. Most people who carry an auto-injector don’t know how to use it correctly. In one study, nearly 7 out of 10 people fumbled the steps during a simulated emergency.
Here’s how to do it right:
- Remove the safety cap - usually a blue or gray tab.
- Place the tip against the outer thigh - through clothing if needed. Don’t hesitate to jab through jeans.
- Push hard until you hear a click. Hold it there for 3 seconds.
- Remove and massage the area for 10 seconds.
That’s it. No twisting. No fiddling. Just jab, hold, and let the medicine do its job. The injection goes into the muscle of the thigh because it’s absorbed fastest - within 8 minutes. If you inject it into fat (like the arm), it takes twice as long to work.
Adults and teens over 30 kg (about 66 lbs) get 0.3 mg. Kids between 15-30 kg get 0.15 mg. Never guess. Use the right dose. If symptoms don’t improve after 5 minutes, give a second dose. Don’t wait. Don’t hope. Give it.
Common Mistakes That Cost Lives
Most people who die from anaphylaxis didn’t get epinephrine in time - not because they didn’t have it, but because they didn’t use it.
Here are the top reasons people delay:
- Thinking it’s just a mild reaction - “It’s only a rash, I’ll wait.”
- Fear of the needle - 1 in 5 people avoid using it because they’re scared.
- Confusion over symptoms - “Is this a stomach bug or anaphylaxis?”
- Waiting for someone else to act - “My spouse has it, I’ll let them use it.”
In one study, 43% of people waited until symptoms got worse before using epinephrine. That’s too late. By then, the body is already shutting down. The rule is simple: if you suspect anaphylaxis, give epinephrine. Then call 911.
What Happens After You Use It
Even if you feel better after the shot, you still need to go to the hospital. Anaphylaxis can come back - sometimes hours later. This is called a biphasic reaction, and it happens in up to 20% of cases. That’s why guidelines now say anyone who needed epinephrine should be observed for at least 12 hours, especially if they have asthma, heart disease, or needed more than one dose.
At the hospital, they’ll check your breathing, blood pressure, and oxygen levels. They might give you more epinephrine, oxygen, or IV fluids. But they won’t give you steroids or antihistamines as the main treatment - because those don’t stop the crisis. They’re just backup.
Choosing and Managing Your Auto-Injector
There are several brands: EpiPen, Auvi-Q, Adrenaclick, and now generics. Auvi-Q has a voice prompt that tells you what to do - “Push here,” “Hold for 3 seconds.” That’s helpful if you’re panicked. EpiPen is the most common, but its instructions are harder to follow under stress.
Cost is a real barrier. In 2023, the average out-of-pocket price dropped to $185 for a two-pack, down from over $300 in 2016. But 30% of people still skip filling their prescription because it’s too expensive. If you’re struggling, ask your doctor about patient assistance programs. Many manufacturers offer free or discounted devices.
Store your auto-injector at room temperature - not in the car, not in the fridge. Heat and cold can ruin the medicine. Check the expiration date every month. Set a phone reminder. Most last 12-18 months. Don’t wait until the last minute to replace it.

Who Needs One - And Who Doesn’t
If you’ve ever had a severe allergic reaction, you need an auto-injector. That includes people with:
- Peanut, tree nut, or shellfish allergies (responsible for 90% of food-related cases)
- Severe reactions to insect stings (bees, wasps, hornets)
- Drug allergies, especially to penicillin
- Latex allergy with past breathing trouble
Even if you’ve only had mild reactions before, if you’ve ever had trouble breathing or a drop in blood pressure, you’re at higher risk for a worse one next time. Doctors recommend auto-injectors for anyone with a history of anaphylaxis - no exceptions.
Parents of young kids with food allergies should carry two - one at home, one at school. Schools in all 50 U.S. states now keep stock epinephrine for emergencies. But if your child has a known allergy, they should have their own.
The Bigger Picture: Why This Matters
More than 1.6% of Americans - over 5 million people - have had anaphylaxis. The number is rising, especially in kids. Peanut allergies tripled between 1997 and 2008. More people are carrying auto-injectors now than ever before. But here’s the problem: 58% of adults can’t even name the key symptoms. Only 37% of people discharged from the ER get a written action plan.
This isn’t just about having a device. It’s about knowing what to do. Training matters. Practice with a trainer pen every month. Teach your family how to use it. Keep one in your bag, your car, your kid’s backpack. If you’re the one with the allergy, don’t assume someone else will help. Be ready.
Epinephrine isn’t perfect. It can cause a racing heart or shaking. But those side effects are far safer than dying. And in the next few years, new tools are coming - smart injectors that text your emergency contacts, longer-lasting versions, and better education programs in schools. But right now, the only thing that saves lives is knowing the signs and acting fast.
What to Do If Someone Else Is Having a Reaction
You don’t have to be the patient to help. If someone collapses, turns pale, can’t breathe, or has swelling around their mouth - act.
- Ask if they have an epinephrine auto-injector.
- If they say yes, help them use it - or use it for them if they’re too weak.
- Call 911 immediately - even if they seem better after the shot.
- Have them lie flat with legs raised, unless they’re having trouble breathing - then let them sit up.
- Stay with them until help arrives.
Don’t wait. Don’t ask if you’re sure. If it looks like anaphylaxis, treat it like anaphylaxis. You could be the reason they live to see tomorrow.
Can antihistamines stop anaphylaxis?
No. Antihistamines like Benadryl may help with itching or hives, but they do nothing to reverse airway swelling, low blood pressure, or shock. Relying on them alone during anaphylaxis can be deadly. Epinephrine is the only treatment that works fast enough to save a life.
How do I know when to use epinephrine?
Use epinephrine at the first sign of a severe reaction - especially if you have trouble breathing, swelling in the throat, dizziness, or a rapid drop in blood pressure. Don’t wait for all symptoms to appear. Skin symptoms like hives or swelling alone aren’t enough to trigger a shot - but if they’re combined with any breathing or circulation problem, act immediately. When in doubt, give it.
Can I reuse an epinephrine auto-injector?
No. Auto-injectors are single-use devices. Once activated, the needle is exposed and the medicine is delivered. Even if you think you didn’t get the full dose, do not try to reuse it. Always carry two, so you have a backup if symptoms return.
Is it safe to use epinephrine if I’m not sure it’s anaphylaxis?
Yes. Epinephrine is very safe when given in the correct dose via the thigh. Side effects like a racing heart or shaking are temporary and far less dangerous than untreated anaphylaxis. If you’re unsure whether it’s a reaction or something else, giving epinephrine is the right call. It won’t hurt you - but not giving it could kill you.
Do I still need to go to the hospital after using epinephrine?
Absolutely. Even if you feel fine after the shot, you need medical care. Anaphylaxis can come back hours later - this is called a biphasic reaction. Hospitals will monitor your vital signs and may give additional treatment. Never skip this step. Your life depends on it.




man i used to think benadryl was the magic bullet until my buddy turned purple at a bbq. epinephrine isn't optional. it's the only thing that doesn't lie.
the pharmacokinetics of intramuscular epinephrine in the vastus lateralis are optimal due to high perfusion and minimal adipose tissue compared to subcutaneous delivery. studies show absorption time is reduced by 47% versus deltoid injection, which is why guidelines mandate thigh administration. also, delayed administration correlates with increased mortality-odds ratio 3.2 in the JAMA study of 2021.
if you're not carrying two pens you're just waiting to die. america's got the best meds in the world but people act like it's a horror movie. get it. use it. don't be a coward.
you guys are literally saving lives with this info 🥹 i used to be terrified of needles but now i practice with my trainer pen every sunday with my kid. we even have a little ritual-‘epi day’-and we high-five after. it’s not just medicine, it’s peace of mind 💪❤️
also, if you’re worried about cost, my doc hooked me up with a free one through the manufacturer program. just ask. you deserve to be safe.
so let me get this straight-someone dies because they waited to see if the hives would ‘get worse’? and we’re still acting like this is normal? 🤦♀️ i’ve seen people text ‘is this anaphylaxis?’ while their kid turns blue. it’s not a poll. it’s a crisis.
no reusing pens dumbass
thank you for writing this. i’ve had two reactions and both times i froze. i didn’t know what was happening until my sister screamed at me to use the pen. since then, i’ve trained my whole family. we even made a checklist taped to the fridge. knowledge isn’t power-it’s survival.
epinephrine is the only thing that works. if you’re still using antihistamines you’re a liability. you’re not just risking your life-you’re risking everyone around you. get educated or get out of the way.