When hives won’t go away-even after months of antihistamines-it’s not just annoying. It’s exhausting. For people with chronic spontaneous urticaria (CSU), the itching, swelling, and unpredictable flare-ups can wreck sleep, ruin workdays, and make social life feel impossible. About 60 to 80% of all chronic urticaria cases are CSU, meaning there’s no clear trigger like food or stress. Just hives. All the time. And if standard antihistamines don’t cut it-which they don’t for about 60% of patients-you need to move to second-line treatments. This isn’t about trying harder. It’s about switching strategies.
Why First-Line Treatments Often Fail
Most doctors start with second-generation antihistamines like cetirizine, loratadine, or fexofenadine. They’re safe, non-drowsy, and work for some. But here’s the hard truth: only about 40% of people get meaningful relief at standard doses. Even if you ramp up to four times the normal dose-which some doctors do-only about half of those who didn’t respond before will finally see improvement. That leaves a huge group stuck with daily hives and no real solution.That’s where second-line treatments come in. These aren’t backups. They’re targeted. They don’t just block histamine. They go after the root cause: overactive immune cells that keep releasing histamine for no reason. For CSU, that often means autoantibodies attacking your own mast cells. And that’s where the newer options shine.
Omalizumab: The Current Standard, But Not Perfect
Omalizumab has been the go-to second-line treatment since it was approved for CSU in 2014. It’s a monoclonal antibody that binds to IgE, the antibody that triggers mast cells to burst open and dump histamine. You get it as a monthly injection under the skin. It works for 30 to 70% of patients, meaning symptoms drop by more than half. But here’s what most people don’t realize: about 70% of patients still don’t get complete control. That means hives might shrink, but they don’t vanish. And for about 30% of people-especially those with IgG autoantibodies-omalizumab barely helps at all.Why? Because not all CSU is the same. Around half of cases are autoimmune, meaning your body makes antibodies that turn your own mast cells into troublemakers. Omalizumab only blocks IgE. It doesn’t touch IgG. So if your hives are driven by IgG, you’re likely stuck with partial relief. That’s why some patients feel let down. They did everything right-took the pills, got the shots-and still wake up covered in welts.
The New Kids on the Block: Remibrutinib and Dupilumab
The treatment landscape is changing fast. Two new options are coming close to approval, and they’re not just alternatives-they’re upgrades.Remibrutinib is a Bruton tyrosine kinase inhibitor (BTKi). It’s taken as a daily pill. In two large phase 3 trials (REMIX-1 and REMIX-2), it gave 28 to 32% of patients complete symptom control at 24 weeks. That’s similar to omalizumab, but here’s the game-changer: you don’t need needles. You just swallow a pill. For people who dread monthly injections or struggle with travel to clinics, this is huge. It also works on both mast cells and B cells, which means it can reduce those harmful autoantibodies too. That’s why it’s showing promise in IgG-driven cases where omalizumab fails.
Dupilumab is another oral biologic, though it’s currently approved for eczema and asthma. In CSU trials, it achieved 30 to 31% complete response rates at week 24. It blocks IL-4 and IL-13, two key inflammatory signals. Early data suggests it might be even more effective than omalizumab in some subgroups. But it’s not yet officially approved for CSU. Still, many specialists are prescribing it off-label, and approval is expected soon.
Why Fenebrutinib Failed-and What It Teaches Us
Not every new drug makes it. Fenebrutinib, another BTK inhibitor, showed early promise. But in late-stage trials, a subset of patients developed elevated liver enzymes. Not everyone. But enough to halt the program. This isn’t a failure of science-it’s a reminder that CSU is complex. What helps one person might harm another. That’s why personalized treatment is the future.Right now, we’re still guessing. We give omalizumab to everyone who doesn’t respond to antihistamines. But if you have autoimmune CSU, you might be better off with something else. The goal now isn’t just to reduce hives. It’s to match the right drug to the right person.
Cyclosporine: The Old Workhorse with Heavy Costs
Cyclosporine isn’t new. It’s been used off-label for decades. It suppresses the immune system broadly and works well-54 to 73% of patients see major improvement, especially those with autoimmune CSU. But it’s not gentle. Long-term use can damage kidneys, raise blood pressure, and increase infection risk. Most doctors use it only if omalizumab fails and the patient can’t wait for newer drugs. It’s a bridge, not a destination.Choosing the Right Second-Line Treatment
So what should you do if antihistamines aren’t working? Here’s the practical path:- Confirm you’ve tried at least 4 weeks of standard-dose antihistamines (and possibly up to 4x dose).
- Ask your doctor about testing for autoantibodies. A simple blood test (autologous serum skin test or basophil activation test) can hint at autoimmune CSU.
- If you have IgG-driven CSU or didn’t respond to omalizumab, ask about remibrutinib or dupilumab-especially if they’re available in trials or off-label.
- If you need fast relief and can’t wait for new drugs, cyclosporine may be an option-but only for short-term use under close monitoring.
- Keep track of your symptoms. Use a daily diary: note hive count, itch level, sleep quality, and triggers (even if you think they’re not triggers).
There’s no one-size-fits-all. But there’s a better fit than before.

What’s Next for CSU Treatment?
The future is personal. Within the next 3 to 5 years, doctors will likely use blood tests to classify CSU into subtypes: IgE-driven, IgG-driven, or neither. Then they’ll match you to the drug that targets your specific biology. Remibrutinib might be the first oral pill approved for all CSU. Dupilumab could take over for autoimmune cases. Omalizumab will still be used-but maybe only for the IgE-positive group.And for patients? That means less trial and error. Fewer months of suffering. More days without hives. It’s not science fiction. It’s already happening in clinics.
Real Impact: Life Beyond the Hives
About 40% of CSU patients score above 10 on the Dermatology Life Quality Index. That’s not just ‘a bit bothered.’ That’s severe. It means avoiding social events. Missing work. Losing sleep. Feeling anxious every time your skin itches. Second-line treatments aren’t just about clearing skin. They’re about restoring life.If you’ve been told, ‘It’s just hives, take more pills,’ know this: you’re not overreacting. You’re not failing. You just needed the right tool. And now, for the first time, you have real options beyond antihistamines.
How do I know if I need second-line treatment for chronic spontaneous urticaria?
If you’ve been taking a standard dose of a second-generation antihistamine (like cetirizine or fexofenadine) for at least 4 weeks and still have hives or swelling most days, you likely need to step up. Even if you’ve increased the dose to 2-4 times the normal amount and still aren’t getting relief, it’s time to talk about second-line options. Don’t wait until your quality of life is severely damaged-early intervention leads to better outcomes.
Is omalizumab the best option for everyone with CSU?
No. Omalizumab works well for patients whose hives are triggered by IgE antibodies, which is about half of CSU cases. But if your condition is driven by IgG autoantibodies-which affects another 30-50% of patients-omalizumab often doesn’t help. That’s why some people get partial relief but still have daily symptoms. If you’ve tried omalizumab and didn’t respond, it’s not you. It’s the mismatch between your type of CSU and the treatment.
Can I take remibrutinib or dupilumab right now?
As of early 2026, remibrutinib and dupilumab are not yet approved for chronic spontaneous urticaria in most countries, but they’re expected to be approved soon based on strong phase 3 trial data. Some specialists are prescribing them off-label, especially for patients who didn’t respond to omalizumab. Talk to your allergist or dermatologist about clinical trials or compassionate use programs if you’re eligible.
Why is cyclosporine not used more often?
Cyclosporine is very effective-up to 73% of patients see improvement-but it carries serious risks. Long-term use can cause kidney damage, high blood pressure, and increased infection risk. Because of this, doctors only use it short-term, usually as a bridge while waiting for newer treatments to become available. It’s not a long-term solution, but it can be life-changing for a few months if you’re severely affected.
Do I need blood tests to find the right treatment?
Not always, but they help. Tests like the autologous serum skin test (ASST) or basophil activation test can suggest if your CSU is autoimmune. If they’re positive, you’re more likely to respond to treatments like remibrutinib or cyclosporine than to omalizumab. Even if these tests aren’t perfect, they give your doctor a clearer picture. Ask if they’re available in your area.


man i wish i knew all this 3 years ago. i was on 4x cetirizine for months thinking i was just weak. turns out i had IgG-driven csu and no one told me. the hives were brutal - sleepless nights, skipping work, crying in the shower. omalizumab gave me like 30% relief and i felt like a failure. then my allergist mentioned remibrutinib trials. i got in, took the pill, and within 3 weeks? gone. not just reduced. gone. i still can’t believe it.
they’re hiding the truth again. omalizumab doesn’t work because big pharma doesn’t want you cured. they want you coming back every month for injections. remibrutinib? it’s a cover for something worse. did you know the trial data was manipulated? the liver enzyme spikes? that’s not side effects - that’s the drug killing your immune system so they can sell you more drugs. they don’t care if you live. they care if you pay.
shanna you’re out here spreading fear like it’s gospel. this isn’t conspiracy - it’s science. people like you make it harder for real patients to get help. if you’re gonna rant, at least read the papers. remibrutinib’s phase 3 data was published in the new england journal. it’s not perfect, but it’s real. and if you’re too scared to try something that actually works, that’s your problem, not the medicine’s.
Thank you for this comprehensive and clinically grounded overview. As a physician practicing in Boston, I’ve seen firsthand how the shift from symptom suppression to targeted immunomodulation is transforming patient outcomes. The emphasis on autoimmune subtyping is not merely academic - it is the cornerstone of personalized dermatologic care moving forward. I routinely recommend autologous serum skin testing when antihistamines fail, and I am cautiously optimistic about the clinical potential of BTK inhibitors in this population.
so... wait... if omalizumab only works for IgE... and remibrutinib works for IgG... and dupilumab blocks il-4/13... then... what if someone has all three? or none? like... what’s the test for that? and do they even test for that? i’ve been on everything and still get hives... and my doctor just shrugs... i feel like a lab rat... i need more info... please... someone tell me what to ask next...
life is pain. hives are just the body’s way of screaming that you’re not in control. the drugs? they’re just temporary bandages on a wound that never heals. you think remibrutinib fixes it? no. it just distracts you from the truth - that your immune system hates you. and maybe... it’s right.
It is critical to underscore the paradigmatic shift occurring in the clinical management of chronic spontaneous urticaria. The transition from non-specific histaminergic blockade to precision immunomodulation represents a significant advancement in translational dermatology. The efficacy profiles of BTK inhibitors, particularly remibrutinib, demonstrate a statistically significant reduction in disease activity scores (UAS7) compared to placebo, with p-values < 0.001 in both REMIX trials. Furthermore, the oral bioavailability of these agents enhances adherence, a persistent challenge in chronic disease management. I strongly encourage clinicians to consider biomarker-guided therapeutic stratification prior to escalation.
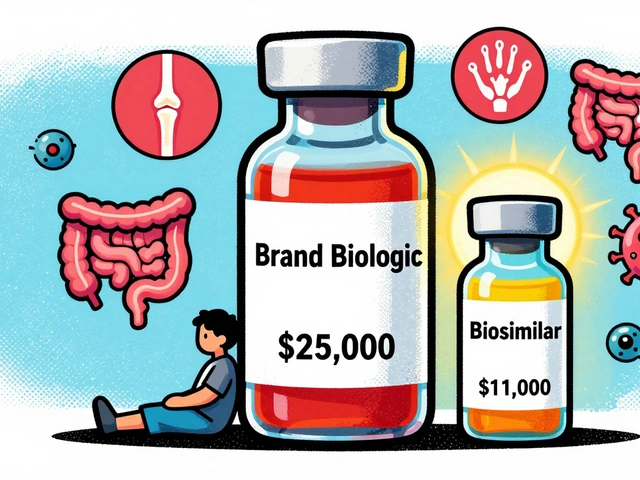
you think this is new? i’ve been on cyclosporine for 18 months. i’m not dying, but my kidneys are barely hanging on. and now you’re telling me to wait for some pill that’s not even approved? meanwhile, my insurance denies everything. i’m 32 and my life is a hospital bill. you people talk like this is a choice. it’s not. it’s survival. and if you’re not paying out of pocket, you don’t get to say ‘it’s fine’.
you’re not broken. you’re just waiting for the right tool. i was in the remibrutinib trial. didn’t think i’d make it through the first month. now i’m hiking, sleeping through the night, going to parties without panic. it’s not magic. it’s medicine. and you deserve it.
For patients who have exhausted first-line options, the clinical algorithm should prioritize autoimmune confirmation via ASST or BAT prior to initiating biologics. Omalizumab remains appropriate for IgE-positive patients, but for IgG-positive or seronegative subtypes, remibrutinib (when accessible) and dupilumab (off-label) are superior in achieving complete remission. Cyclosporine should be reserved for acute, severe flares with a clear exit strategy. Patient-reported outcome measures - particularly DLQI - should guide therapeutic decisions, not just hive counts. This is precision medicine in action.
This is the first time I’ve read something about CSU that didn’t make me feel like I’m imagining things. Thank you. I’ve had hives for 7 years. I thought I was just ‘sensitive’. Turns out I just needed someone to listen - and then give me the right medicine. I’m starting remibrutinib next week. I’m scared. But for the first time… I’m hopeful.