Every year, people get the wrong medicine-not because of a mistake in the prescription, but because two drugs look or sound too much alike. It’s not rare. It’s not an accident. It’s a system failure that’s been hiding in plain sight for decades. In the U.S., one in four medication errors comes from confusing similar drug names. That’s not a glitch. That’s a pattern. And it’s killing people.
What Exactly Are Look-Alike, Sound-Alike (LASA) Medications?
Look-alike, sound-alike (LASA) medications are drugs that are easily mistaken for each other because their names look similar on paper or sound alike when spoken. This isn’t just about spelling. It’s about how the brain processes information under pressure. Take HYDROmorphone and hYDROcodone. Both are painkillers. Both end in “-done.” But one is ten times stronger than the other. Give the wrong one to a patient, and you could cause a fatal overdose. The FDA started using tall man lettering-capitalizing the different parts of the name-to help. But if you’re tired, rushed, or working a double shift, those capital letters don’t always stick out. Then there’s simvastatin 10 mg and simvastatin 20 mg. Same drug. Different strength. But in a busy pharmacy, with dozens of bottles on the shelf, the difference in the number can be missed. A 2022 study found this pair was the most common source of LASA errors in hospitals. Even worse: doxorubicin and daunorubicin. Both are chemotherapy drugs. Both are red. Both are given through IV. Mistake one for the other, and you’re not just giving the wrong dose-you’re giving a toxic overdose that can stop a heart.Where Do These Errors Happen?
Most people think errors happen in the pharmacy. But they don’t. They start earlier.- Prescribing (24%): A doctor writes “Lovenox” but means “Heparin.” Both are blood thinners. Both are written in haste.
- Transcribing (15%): A nurse hears “Zyrtec” over the phone but writes “Zyprexa.” One’s for allergies. The other’s for schizophrenia.
- Dispensing (21%): A pharmacist grabs the wrong bottle from the shelf. The labels are nearly identical. The colors match. The font is the same.
- Administration (68%): This is where the damage happens. A nurse reaches for the vial labeled “Versed” but pulls out “Vecuronium.” One calms a patient. The other paralyzes them. If you don’t double-check, the patient can’t breathe.
Why Do These Mistakes Keep Happening?
The problem isn’t just the names. It’s the system. Pharmacies and hospitals use hundreds of drugs. New ones are approved every year. Drug companies pick names that sound catchy, marketable, or easy to pronounce. They don’t always ask: “Will this confuse someone in a rush?” The FDA has denied 34 new drug names since 2022 just because they were too similar to existing ones. But that’s only new drugs. What about the 5,000+ already on the market? Many were approved before anyone thought to check for confusion. Even when hospitals try to fix it, the fixes often fall short. Tall man lettering (like CELEBREX vs. CELEBREX) helps-but only if staff know what it means. A 2022 review found it creates a “quasi-placebo effect.” People think it works because they’ve seen it, not because it actually prevents errors. And then there’s workload. During shift changes, night shifts, or busy holidays, pharmacists and nurses are running on fumes. A 2022 study found anticipatory errors spike during high-stress moments. Someone grabs a bottle because it “looks right.” They don’t read the label. They assume.
High-Alert Medications Are the Deadliest
Not all LASA errors are equal. Some are dangerous. Others are just inconvenient. The most lethal mix-ups involve high-alert medications:- Insulin (regular vs. long-acting)
- Opium-based painkillers (morphine vs. hydromorphone)
- Anticoagulants (warfarin vs. enoxaparin)
- Neuromuscular blockers (vecuronium vs. versed)
- Chemotherapy drugs (doxorubicin vs. daunorubicin)
What’s Being Done to Fix This?
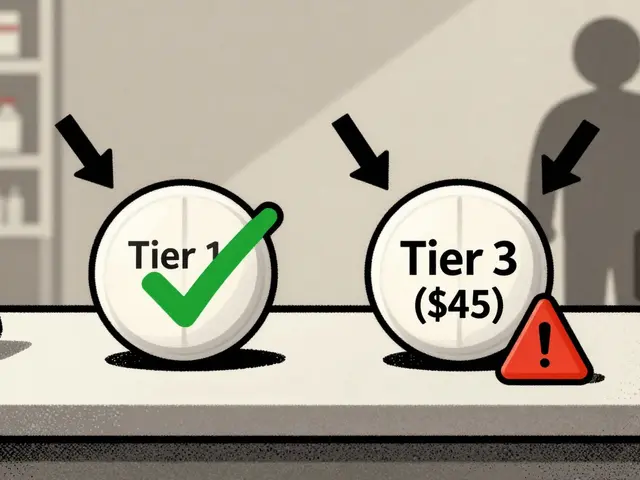
Some hospitals are getting smarter.- Tall man lettering is used on over 200 drug pairs in the U.S. It’s not perfect, but it’s better than nothing.
- Electronic prescribing systems now flag LASA pairs. Epic’s SafeMed module reduced errors by 28.7% in a 12-hospital trial.
- Moveable signage in pharmacies highlights high-risk pairs. One hospital put up a bright yellow sign that reads: “DO NOT CONFUSE: HYDROmorphone / hYDROcodone.” It’s simple. It works.
- AI voice recognition is being tested at Johns Hopkins. The system listens to verbal orders and flags confusing names in real time. Early results? 89.3% accuracy.
What You Can Do-Even If You’re Not a Doctor
You don’t have to be a healthcare worker to help stop these errors.- Always ask: “What is this medicine for?” If the answer is vague-“It’s for your heart”-dig deeper.
- Check the label: Does the name match what your doctor said? Does the strength match your prescription?
- Speak up: If something looks off, say something. “I thought this was 5 mg, not 10 mg.”
- Know your meds: If you take insulin, blood thinners, or chemotherapy, memorize the exact name and strength. Don’t rely on the bottle.
The Future: Can We Really Stop This?
There’s hope. The FDA is pushing for mandatory testing of all new drug names using algorithms based on the Lesar study-a model that predicts confusion risk with 95% accuracy. If approved, no new drug can enter the market without passing a “confusion test.” The International Pharmaceutical Federation wants global standards for drug naming and packaging by 2030. Imagine pills and vials designed so you can’t confuse them-even in the dark. Dr. Donald Berwick from NEJM says we could cut LASA errors by 80% in ten years. That’s ambitious. But possible-if we treat this like a public safety issue, not just a medical one. Right now, it’s a patchwork. Some hospitals have systems. Others don’t. Some staff are trained. Others aren’t. The difference between life and death often comes down to whether someone paused for five seconds to check the label.What’s the Bottom Line?
Look-alike, sound-alike drug errors aren’t accidents. They’re predictable. They’re preventable. And they’re happening right now-in hospitals, clinics, and pharmacies near you. The system isn’t broken. It’s just lazy. We’ve known about this for 25 years. We have the tools. We have the data. What we’re missing is the will. Next time you pick up a prescription, don’t assume it’s right. Look. Ask. Confirm. You might just save a life.What are the most common look-alike, sound-alike drug pairs?
The most frequent pairs include: HYDROmorphone/hYDROcodone, doxorubicin/daunorubicin, simvastatin 10 mg/simvastatin 20 mg, levoTHYroxine/SYNTHROID, vecuronium/versed, and naltrexone/naloxone. These are flagged by the ISMP and FDA as high-risk. Even small differences in spelling or strength can lead to serious errors.
Is tall man lettering effective at preventing these errors?
Tall man lettering (like HYDROmorphone vs. hYDROcodone) helps-but only if staff understand its purpose. Studies show it creates a “quasi-placebo effect.” It reduces errors modestly, but not reliably. It’s a tool, not a solution. It works best when combined with electronic alerts, training, and double-checking.
Why do these errors happen more often at night or during shift changes?
Fatigue, distractions, and rushed transitions make people rely on shortcuts. During night shifts or handoffs, staff are more likely to grab a bottle because it “looks familiar” instead of reading the label. A 2022 study found anticipatory errors spike during these times-especially when workload is high and sleep-deprived.
Can AI really help prevent LASA errors?
Yes. Early AI systems that listen to verbal medication orders and flag confusing names have shown 89.3% accuracy in trials at Johns Hopkins. These tools don’t replace human judgment-they give staff a second chance to catch mistakes before they happen. They’re especially useful in fast-paced environments like ERs and ICUs.
What should I do if I think I received the wrong medication?
Don’t take it. Call your pharmacist or doctor immediately. Compare the name and strength on the label to your prescription. If they don’t match, ask for clarification. If you’re unsure, ask for the medication’s purpose. If the answer doesn’t make sense, hold off. It’s better to delay a dose than risk a life-threatening error.
Are LASA errors more common in certain types of hospitals?
Yes. Hospitals with over 200 beds are 72% more likely to have formal LASA prevention programs than smaller facilities. Resource-limited clinics and rural pharmacies often lack electronic alerts, trained staff, or updated signage. That’s why errors are more common in these settings-even though the same drugs are used everywhere.


This is so real I could cry. Saw a nurse almost give vecuronium instead of versed on my mom’s shift-she caught it because she paused. Just pause. Always pause. ❤️
I work triage in a rural ER. We don’t have electronic alerts. We have sticky notes on the fridge that say ‘HYDROmorphone ≠ hYDROcodone’ in Sharpie. It’s not enough-but it’s what we’ve got. We’re all just trying not to kill someone today.
The epistemological failure here is systemic: the conflation of pharmacological semiotics with marketing pragmatics has produced a lethal ontological ambiguity in therapeutic nomenclature. The FDA’s tall-man lettering is a syntactic bandage on a hemorrhagic wound. We’re not fixing nomenclature-we’re optimizing for cognitive load reduction under duress, which is a behavioral engineering problem, not a regulatory one. The root cause? Capitalism’s colonization of medical taxonomy. Drug names aren’t designed for safety-they’re designed for brand recall. We’re medicating in a linguistic minefield because profit margins outweigh patient survival curves.
THIS IS ALL A COVER-UP!!! The pharmaceutical companies KNOW about this-they’ve been doing it on purpose since the 90s!!! They want you to mix up the drugs so you need MORE drugs!!! They’re working with the FDA!!! They even make the bottles look the same on purpose!!! My cousin died because of this!!! WHY ISN’T THIS ON THE NEWS???!!!
So many people don’t realize how much this affects everyday folks like me. I take insulin and I always check the label three times even though I’ve been on it for 12 years because one time I almost grabbed the wrong pen and I just froze I didn’t know if I was being paranoid or not but better safe than sorry right I mean what if I’d given myself 50 units instead of 10 what would have happened I don’t even want to think about it but now I carry a laminated card with my meds on it and I show it to every nurse and I say hey this is mine and they always look at me funny but I don’t care because I’m alive and that’s what matters
In India, we don’t have tall-man lettering. We have handwritten scripts. And yet, pharmacists still get it right 95% of the time. Culture matters more than tech.
I’m a nurse. I’ve had two near-misses. One with levothyroxine and Synthroid. One with morphine and hydromorphone. I don’t blame the system. I blame the silence. We need to stop pretending this is just ‘human error.’ It’s a design flaw. And we’re all just trying to survive it.
They’re not just mixing up drug names-they’re mixing up your DNA. The real story? The FDA is in bed with Big Pharma. They’re using LASA errors to justify mandatory RFID chips in every pill. That’s why they won’t fix the names. They want you dependent. They want you tracked. They want you to think it’s an accident. It’s not. It’s the next step in the Great Medical Control Grid. Wake up.